Supervised by: Amanda Liu, BEng, MSc. Amanda spent her undergraduate years studying Biochemical Engineering at UCL (University College London), where she was awarded First Class Honours. She then completed her Master’s degree in Clinical and Therapeutic Neuroscience at the University of Oxford. She is currently studying Medicine (Graduate Entry) at the University of Cambridge.
Introduction
The COVID-19 pandemic and lockdown have impacted the lives of people all over the world. Its unprecedented nature has produced feelings of anxiety, fear, and uncertainty in both adults and children, while simultaneously altering life as people knew it. To combat the spread of infection, many countries have resorted to social distancing and isolation. They enforced such strategies by implementing national lockdowns. Complying with these containment measures, school closures became widespread, extracurricular activities and sports were cancelled, and contact with friends or extended family was strongly discouraged. Under these strict and difficult circumstances, many children and adolescents found themselves feeling more stressed, anxious, depressed, lonely, and helpless than before. Despite limited longitudinal studies on the matter, those available have suggested that COVID-19 has led to perceived increases in anxiety, loneliness, depression, and emotional distress alongside decreases in life satisfaction (Magson et al., 2020; Bignardi et al., 2020). Other studies have confirmed these findings and predicted that the pandemic will continue to adversely affect today’s children and adolescents. The extent of such effects are in part dependent on many factors, such as whether the young person is economically underprivileged, has special needs, is separated from parents, has preexisting mental health conditions, or is of female sex. With the increasing fragility of children and adolescent’s mental health and the unpredictability of the future of the COVID-19 pandemic, it is imperative that proper interventions are implemented to ensure the psychological needs of our youth are being taken into consideration.
This paper is designed to review multiple pieces of primary scientific literature related to the effect of COVID-19 on children and adolescent’s mental health and determine how children and adolescents can be best accommodated during these trying times.
Material and Methods
The databases of PubMed, Science Direct, and Google Scholar were searched to obtain articles relevant to COVID-19 and child/adolescent mental health. Queries such as “COVID-19 and child/adolescent mental health” were searched. Upon finding the articles, I analyzed them and sorted them into one of the following headings: Effect on the Economically Underprivileged, Effect of Quarantine and Separation from Parents, Effect on Having Special Needs, Effect on Females vs Males, Comparison to Past Epidemics and Outbreaks, and Potential Interventions.
Effect of COVID-19 on the Economically Underprivileged
For a long time, economic and social inequalities have been a risk factor in developing mental health problems. This issue has been exacerbated by the COVID-19 pandemic and its related lockdowns and unemployment. With facilities closing and people being forced to stay home, many families have found themselves struggling to stay afloat. In the United States alone, 31.3 million people reported in July that they were unable to work because the COVID-19 pandemic caused their employer to shut down business (Bignardi et al., 2020). The issue with being economically disadvantaged and being at greater risk of mental health issues, however, is most prominent in developing countries where more children now face prolonged stress due to a lack of nutrition and safety (essential aspects of life that a salary can generally provide for). In India (home to 472 million children), for example, 40 million children from lower socioeconomic families have been significantly affected. These include street children, farm children, and migrant children (Dalton et al., 2020; Rosenthal et al., 2020). This population of children and adolescents come from families that no longer have a steady source of income, making them more vulnerable to abuse and the mental health problems that come with it (Birla, 2019). The reasoning for increased susceptibility to abuse is that a lack of parental income has been shown to induce feelings of helplessness or frustration which can manifest themselves in the form of violence. Such violence then increases a child’s risk of suicide, depression, or anxiety. (Jiao et al., 2020; Petito et al., 2020; Solantaus et al., 2004). Child abuse is also an imminent risk during the COVID 19 pandemic because lockdowns, school closures, and an interruption in social services give children no escape from their home lives. (Cooper, 2020; United Nations, 2020). The threat of child abuse in times of viral outbreaks or epidemics is a pattern that has been seen before, for example in the 2014-2016 Ebola outbreak in West Africa, where school closures resulted in increases in child labor, sexual abuse, neglect, and teenage pregnancies (Cooper, 2020). The announcement from the Deputy Director of ‘CHILDLINE 1098’ India that there has been a 50 percent increase in helpline calls since the start of the lockdown supports the correlation between COVID-19 lockdowns and the increased abuse of underprivileged children (PTI, 2020).
Besides the mental health problems caused by abuse or violence, the mental health of economically underprivileged children and adolescents has also been affected by COVID-related educational changes (online classes, distance learning, etc). Because of these changes, many underprivileged children and adolescents haven’t been able to access the education they need. Without the stimulation and social interaction that school provides, these children and adolescents are even more at risk of detrimental mental and psychological effects.
Effect of Quarantine and Separation from Parents
In addition to mass lockdowns and social distancing guidelines as preventative measures, many countries have created stricter regulations in the case of infection, most of which consist of total isolation. While complete isolation does serve its purpose of containing the spread of the SARS CoV-2 virus, it likely harms the mental health of those in isolation as well as their families. Generally, when one member of a family contracts the virus, other members are most likely to contract it next. Consequently, a positive COVID test is usually enough to warrant a whole family quarantining from the public and from each other. Such familial separation, especially in the case of a child or adolescent being separated from their parents, can lead to serious mental health consequences as the child or adolescent endures sadness, fear of death, anxiety, fear of parent’s death, and fear of hospitalization. This psychological threat that comes from separation from parents and quarantine aligns with previous research regarding the separation of a primary caregiver and increased psychological detriment (Seijo et al., 2016).
Aside from children being separated from parents in the case of infection, many children that started virtual schooling from home and were separated from their parents on the weekdays also proved to be at a greater risk for mental health problems, specifically anxiety and depression. One study conducted via an online questionnaire available to adolescents in Guiyang, China found that, of the 1036 questionnaires that met the admittance criterion for subsequent analysis, there were 112 (11.78%) cases with depression, 196 (18.92%) cases with anxiety, and and 68 (6.56%) cases with both depression and anxiety reported. Upon further analysis (specifically logistic regression analysis), the study concluded that “companion on weekdays”, education of parents, age, gender, and physical exercise were associated with depression while “companion on weekdays”, gender, and physical exercise were associated with anxiety (see graph below for these results) (Chen et al., 2020). The fact that “companion on weekdays” proved to be a relevant factor implicated in the prevalence of both depression and anxiety suggests that the separation of children and adolescents from parents during the pandemic may have a causal relationship with anxiety and depression rates amongst children and adolescents. This result also supports other studies that have shown parents play an important role in influencing the mental health of children following some sort of disaster (Cobham et al., 2016).
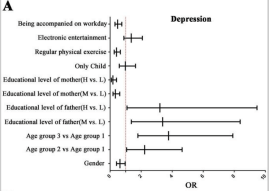
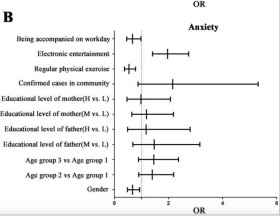
Anything within the dotted red line is considered a risk factor associated with the disorder. “Being accompanied on workday” is associated with both anxiety and depression.
Effect of COVID-19 on Children/Adolescents with Special Needs
One particular population of children and adolescents that has been particularly hard hit by the COVID 19 pandemic are those with special needs. These children are known to be most successful when accommodated to a specific daily routine. Predictability in their environment and activities reduces problematic behaviors as well as anxiety. Thus, the uncertainty of the COVID-19 pandemic and transition to a time of lockdown has proven to be especially challenging for these children (CDC, 2020). In addition to a disruption in daily routine, many special needs children cannot comprehend the complexity of the pandemic and struggle to access the resources they need (psychologists, peer groups, etc) to adapt.
A specific example highlighting the negative effect of the COVID-19 pandemic on the mental health of children and adolescents with special needs is a study entitled “The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder”. This study consisted of two groups of OCD patients (ages 7-21). The first group was recently diagnosed in a specialized OCD clinic in the Central Denmark Region (the CG) while the second group was found through the Danish OCD Association (the SG). This study found that 44.6% reported a worsening of their symptoms in the CG, with 33.8% reporting a worsening of depressive symptoms, 32.3% reporting a worsening of anxiety, 11 participants reporting a worsening of depression and anxiety, and 18.5% reporting an increase in avoidance behavior. In the SG, 73% reported a worsening of their symptoms, with 43.2% reporting a worsening of depressive symptoms and 54.1% reporting a worsening of anxiety (Nissen, 2020). (See data tables below for full results). These results clearly suggest a positive correlation between increasing anxiety/depression symptoms and worsening OCD. They also indicate that COVID played a role in the worsening of symptoms. The strengths of this study are that it consisted of two groups which both showed the same trend and it had a strong response rate. A limitation, however, is that the questionnaire used for the study was self-rated and non-validated.
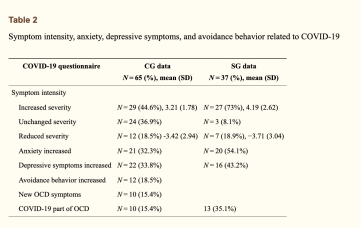
The increase in anxiety and depressive symptoms are seen in rows 5 and 6 of the data table above.
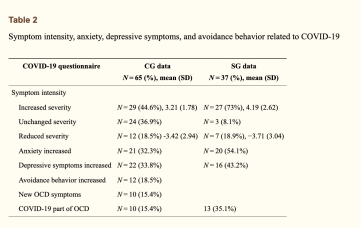
This table shows how anxiety and depressive symptoms have been linked to COVID-19.
While in the case of the OCD study, the COVID-19 pandemic was suggested to have a negative impact on the mental health of children and adolescents with special needs, it is important to note that having some type of disorder does not always lead to elevated mental health issues compared to the general child population. A recent study on the “Effect of the COVID-19 pandemic among children with cystic fibrosis and their mothers” found that, while the COVID-19 pandemic may increase anxiety among the mothers of children with cystic fibrosis, there is no evidence to suggest that COVID-19 affects the anxiety of children with cystic fibrosis any more than it affects the anxiety of other children. (See date table below) (Senkalfa et al., 2020).
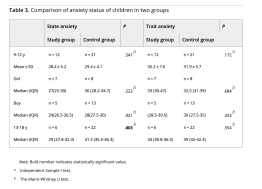
There is not a significant difference between the study group and control group for state anxiety or trait anxiety when the margin of error is taken into consideration
Effect on Females vs Males
While most studies have generally shown that the COVID-19 pandmeic has affected the mental health of both female and male children/adolescents, many studies have indicated that the female sex may be affected to a greater extent. A systematic review and metaanalysis study based on 23 studies with 57,927 children and adolescents found that the prevalence of depression and anxiety were 29% and 26%, respectively. The subgroup meta-analysis of depression then revealed that the prevalence of depression in males (28.9%, 95%CI: 14.1%, 43.7%, p<0.001) was lower than the prevalence of depression in females (33.9%, 95%CI: 24.6%, 43.1%, p<0.001). Similarly, the prevalence of anxiety in males (22.3%, 95%CI: 14.2%, 30.4%, p<0.001) was lower than the prevalence of anxiety in females (27.4%, 95%CI: 20.3%, 34.6%, p<0.001) (See table below) (Ma et al., 2021). These results suggest that being female might be an additional risk factor in adolescents developing mental health or psychological issues. A limitation of this meta-analysis study, however, is that the studies it included were all conducted in China. This makes it difficult to generalize the findings to other countries or the world population. A second limitation to note is that most of the studies analyzed used non-probability sampling and online surveys, which reduces chances of the sample being representative and thereby generalizable. Thirdly, although there was overlap in the tests the studies used to assess anxiety, depression, sleep disorders, and post-traumatic stress, the cut off scores of these tests varied from study to study. The different tests used and the different cut offs for those tests causes one to question the accuracy and reliability of the results. Nevertheless, considering the limited number of studies available, this study still provides useful insight into the impact of gender differences on the effect of COVID-19 on mental health. The finding of there being a higher prevalence of anxiety and depression in females is also plausible considering it aligns with pre-COVID research that established a gender gap in depressive and anxiety symptoms (Ma et al., 2021).
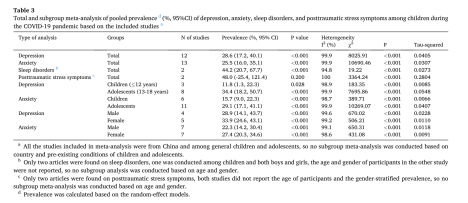
The disparity of prevalence in females vs males is observable in the last four rows of the data table. The prevalences listed in this four rows all have a p-value of less than 0.001 meaning there is 99.999% confidence that the results are not due to randomness or chance.
It is important to note that other systematic studies (Vindegaard & Benros, 2020) have reinforced the association between being female and being more likely to have mental health issues as a result of the COVID-19 pandemic. A study entitled “COVID-19 pandemic and mental health consequences: Systematic review of the current evidence” consisting of 43 studies found that post traumatic stress syndrome is associated with the female gender, as are low psychological well-being or psychiatric symptoms in general. Likewise, to the previous study, a main limitation of this one is that all but four of the studies it included were conducted in Asia (which again compromises the study’s generalizability).
Comparison to Past Epidemics and Outbreaks
Compared to past outbreaks and pandemics, the COVID-19 pandemic is often considered to be much larger in scale. Thus, one would expect the effect of COVID-19 on child and adolescent mental health to be greater than the effect of past pandemics on mental health. Some studies suggest this is true. For example, a study conducted in China found that 40.4% of participants reported having psychological problems during the COVID-19 pandemic compared to 26.2% in the SARS period (Liang et al., 2020). The limitation of this data, however, is that it does not account for other factors or confounding variables that may have led to the increase in percentage. For instance, mass media, misinformation, daily stressors, the world political climate, etc. have all changed from the time of SARS to now. This natural evolution of society may be responsible for the disparity in the percentage of participants having psychological problems during two different times of a viral pandemic as opposed to the nature of the pandemics themselves.
Despite comparison studies between COVID-19 and past pandemics being unable to account for other variables, there are studies that still show similarities over time. In one study, Norwegian researcher SvennErik Mamelund studied the situation of asylums in Norway between 1872 and 1929 and discovered that many Spanish Flu survivors developed difficulty adapting to certain environments, attention disorders, sleep disorders, and depression (Luca et al., 2020). Although this study doesn’t focus specifically on the mental health of children and adolescents, it still draws an interesting parallel between the COVID-19 pandemic and the Spanish Flu pandemic (which is considered to be the only pandemic comparable to COVID-19 in terms of its scope). Both pandemics suggest a relationship between a pandemic and increased mental health problems. Seeing as COVID-19 research shows that both adults and children have been similarly affected in certain ways, one can hypothesize that children were also affected similarly to adults in the Spanish Flu. A lack of evidence from the era of the Spanish Flu pandemic makes this hypothesis difficult to ever prove correct, however.
Potential Interventions
With many vulnerability factors in children and adolescents developing mental health problems, it is essential that interventions be implemented to address these factors and give today’s youth the best chance of surviving the COVID-19 pandemic with the least possible long-term detriment. To address the first vulnerability factor discussed in this paper, the economically underprivileged can be safeguarded by having pediatricians provide affordable teleconsultations with their patients. Not only will this give children’s parents an opportunity to understand what their child is going through, but it can also give the child a chance to report any instances of domestic violence or abuse. Offering free online educational programs to children in developing countries can also help keep them stimulated and reduce the chances of psychological problems. To address the second vulnerability factor of separation from parents, this can be settled by encouraging parents to educate their children about the pandemic while limiting exposure to news in order to prevent anxiety (Wang et al., 2020), having parents’ model appropriate coping mechanisms and preventative measures, having parents provide as stable of a routine as possible, and educating parents about how to stay safe and limit chances of the need quarantine. To address the third vulnerability factor of having special needs, this can be best managed by engaging children in tele-therapy, providing psychoeducation to parents, and having diagnostic and psychological assessment tools available (the earlier a diagnosis is made, the earlier a child can be appropriately treated). In general, parents, teachers, counselors, pediatricians, and any other adult role model involved in a child or adolescent’s life, should simply consider and even prioritize mental health when making decisions or just in everyday life.
Conclusion
With the large amount of evidence supporting the negative affect COVID 19 has had on the mental health of children and adolescents as well as historical pandemic trends, it is clear that there is a pressing need for interventions to cater to the psychological wellbeing of today’s youth (especially those having one or more of the risk factors previously discussed). Children and adolescents not only need to be taught proper coping mechanisms, but they also need collaboration among parents, psychologists, psychiatrists, pediatricians, and community volunteers who can provide them with the support and services they need during this difficult time.
Bibliography
Bignardi, G., Dalmaijer, E. S., Anwyl-Irvine, A. L., Smith, T. A., Siugzdaite, R., Uh, S., & Astle, D. E. (2020). Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Archives of Disease in Childhood, 106(8), 791–797. https://doi.org/10.1136/archdischild-2020-320372
Birla, N. (2019, September 10). Mental health may hurt India to tune of $1.03 trillion; here’s a dose for cos. Economic Times. https://economictimes.indiatimes.com/magazines/panache/mental-health-may-hurt-india to-tune-of-1-03-trillion-heres-a-dose-for-cos/articleshow/71045027.cms
CDC. (2020, June 15). Data and statistics on children’s mental health. Centers for Disease Control and Prevention. https://www.cdc.gov/childrensmentalhealth/data.html Chen, F., Zheng, D., Liu, J., Gong, Y., Guan, Z., & Lou, D. (2020). Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain, Behavior, and Immunity, 88, 36–38. https://doi.org/10.1016/j.bbi.2020.05.061
Cobham, V. E., McDermott, B., Haslam, D., & Sanders, M. R. (2016). The role of parents, parenting and the family environment in children’s post-disaster mental health – PubMed. Current Psychiatry Reports, 18(6). https://doi.org/10.1007/s11920-016-0691-4
Cooper. (2020). Don’t let children be the hidden victims of COVID-19 pandemic. https://www.unicef.org/press-releases/dont-let-children-be-hidden-victims-COVID-19- pandemic
Dalton, L., Rapa, E., & Stein, A. (2020). Protecting the psychological health of children through effective communication about COVID-19. The Lancet. Child & Adolescent Health, 4(5), 346–347. https://doi.org/10.1016/S2352-4642(20)30097-3
Jiao, W. Y., Wang, L. N., Liu, J., Fang, S. F., Jiao, F. Y., Pettoello-Mantovani, M., & Somekh, E. (2020). Behavioral and emotional disorders in children during the COVID-19 epidemic. The Journal of Pediatrics, 221, 264-266.e1. https://doi.org/10.1016/j.jpeds.2020.03.013
Liang, Ren, Cao, Hu, Qin, Li, & Mei. (2020). The effect of COVID-19 on youth mental health. Psychiatric Quarterly, 91(3), 841–852. https://doi.org/10.1007/s11126-020-09744-3 Luca, L., Baroiu, L., Ciubara, A. B., Anghel, R., Bulgaru-Iliescu, A. I., Anghel, L., & Ciubara, A. (2020). COVID-19 and the spanish flu. From suffering to resilience. BRAIN. Broad Research in Artificial Intelligence and Neuroscience, 11(3sup1), 01–07. https://doi.org/10.18662/brain/11.3sup1/116
Ma, L., Mazidi, M., Li, K., Li, Y., Chen, S., Kirwan, R., Zhou, H., Yan, N., Rahman, A., Wang, W., & Wang, Y. (2021). Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Affective Disorders, 293, 78–89. https://doi.org/10.1016/j.jad.2021.06.021
Magson, Freeman, Rapee, Richardson, Oar, & Fardouly. (2020). Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 Pandemic. Journal of Youth and Adolescence, 50(1), 44–57. https://doi.org/10.1007/s10964-020- 01332-9
Nissen, J. B. (2020). The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder.
Petito, A., Pop, T. L., Namazova-Baranova, L., Mestrovic, J., Nigri, L., Vural, M., Sacco, M., Giardino, I., Ferrara, P., & Pettoello-Mantovani, M. (2020). The burden of depression in adolescents and the importance of early recognition – PubMed. The Journal of Pediatrics, 218. https://doi.org/10.1016/j.jpeds.2019.12.003
PTI. (2020, April 8). Govt helpline receives 92,000 calls on abuse and violence in 11 days. Economic Times. https://economictimes.indiatimes.com/news/politics-and-nation/govt helpline-receives-92000-calls-on-abuse-and-violence-in-11- days/articleshow/75044722.cms?utm_source=contentofinterest&utm_medium=text&utm _campaign=cppst
Rosenthal, D. M., Ucci, M., Heys, M., Hayward, A., & Lakhanpaul, M. (2020). Impacts of COVID-19 on vulnerable children in temporary accommodation in the UK. The Lancet. Public Health, 5(5), e241–e242. https://doi.org/10.1016/S2468-2667(20)30080-3
Seijo, D., Fariña, F., Corras, T., Novo, M., & Arce, R. (2016). Estimating the epidemiology and quantifying the damages of parental separation in children and adolescents. Frontiers in Psychology, 0. https://doi.org/10.3389/fpsyg.2016.01611
Senkalfa, B., MD, Eyuboglu, T., MD, Aslan, A., MD, Gursoy, T., MD, Soysal, A., PhD, Yapar, D., MD, & İlhan, M., MD, PhD. (2020, June 12). Effect of the COVID-19 pandemic on anxiety among children with cystic fibrosis and their mothers. https://doi.org/10.1002/ppul.24900
Singh, S., Roy, D., Sinha, K., Parveen, S., Sharma, G., & Joshi, G. (2020). Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Research, 293, 113429. https://doi.org/10.1016/j.psychres.2020.113429
Solantaus, T., Leinonen, J., & Punamaki, R.-L. (2004). Children’s mental health in times of economic recession: Replication and extension of the family economic stress model in Finland – PubMed. Developmental Psychology, 40(3). https://doi.org/10.1037/0012-1649.40.3.412
United Nations Policy brief: the impact of COVID-19 on children. United Nations. 2020:1–17. Policy brief]
Vindegaard, N., & Benros, M. (2020). COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity, 89, 531–542. https://doi.org/10.1016/j.bbi.2020.05.048
Wang, W., Xu, Y., Gao, R., Lu, R., Han, K., Wu, G., & Tan, W. (2020). Detection of sars-cov-2 in different types of clinical specimens. JAMA, 323(18), 1843–1844. https://doi.org/10.1001/jama.2020.3786