Supervised by: Rita Kimijima-Dennemeyer, BA (Hons). Rita recently graduated from the University of Oxford having read Psychology, Philosophy, and Linguistics. She has a particularly interest in clinical psychology, mental health policy, and the ethics of mental health treatment, and she intends to pursue a masters degree in this field.
Abstract
The COVID-19 crisis can be increasingly devastating for patients that live with mental conditions. This study plans to determine if patients with attention deficit hyperactivity disorder (ADHD), post-traumatic stress disorder (PTSD), and depression experienced worsened symptoms during this pandemic. We reviewed twelve articles discussing ADHD, PTSD, or depression, including interviews and peer-reviewed studies. Overall, the majority of peer-reviewed papers indicate a worsening of symptoms in patients with ADHD, PTSD, and depression during the COVID-19 pandemic. We also identify risk factors for each group, respectively, and discuss trends found throughout the studies. For ADHD, the main risk factors for increased symptoms are lack of control and feeling unsafe and/or fearful. For PTSD, risk factors include the fear of losing loved ones, catching the virus, shorter sleep durations, social isolation, fear of disease, and financial insecurity. For depression, they include a low income, feeling out of control, and having a lack of social interaction. Future directions for research on this topic include review papers dedicated to each condition, including an analysis of the initial severity of the condition and its impact on the worsening of symptoms.
Introduction
Though COVID-19 is now a threat to public health and society worldwide, there is a striking lack of research into vulnerable populations, and particularly those with pre-existing mental conditions. The media has mainly focused on the effect of the pandemic on the general population’s mental health, while overlooking those with pre-existing mental conditions. Cullen et al. (20020) argue that “During an outbreak of an infectious disease, the population’s psychological reactions play a critical role in shaping both spread of the disease and the occurrence of emotional distress and social disorder during and after the outbreak” (Cullen et al., 2020). We aimed to investigate whether individuals with pre-existing mental conditions prior to the COVID-19 pandemic experienced a worsening of their symptoms and what key factors are associated with such phenomena. While research is sparse with regards to psychiatric disorders in viral pandemics, we hypothesized that difficulty in managing uncertainty, in general, can worsen a psychiatric patient’s symptoms or prompt the onset of new symptoms.
During the COVID-19 outbreak, individuals with mental conditions have been neglected despite their suffering. A recent study reviewed how individuals with mental conditions have been overlooked and stigmatized during the pandemic (Moore et al., 2020). The study looked at how individuals with mental conditions might be more susceptible to contracting the virus partly due to neglect. One study that reported 50 cases of COVID-19 among individuals with mental conditions in Wuhan, China, has raised concern over this issue (Yao et al., 2020). Reasons for psychiatric patients’ high susceptibility to the virus include cognitive impairment, lack of awareness of risk, caregivers not protecting patients, and confined conditions in psychiatric wards. The authors also argue that those with serious mental illnesses such as schizophrenia, “could experience greater susceptibility to emotional responses to the pandemic, such as fear, anxiety, stress, depression, as well as risk of relapse or worsening of positive (e.g., paranoia, hallucinations) … and negative (e.g., anhedonia, apathy) psychotic symptoms.” Some of the reasons for these occurrences include higher stress responses, lack of access to resources for continued mental health services, reduced job or food security, and additional restrictions in situations such as group homes. We might discover similar risk factors for the conditions we are investigating in this review paper.
Pre-existing psychiatric conditions that may make individuals more vulnerable to worsening symptoms during the COVID-19 pandemic are attention deficit hyperactivity disorder (ADHD), post-traumatic stress disorder (PTSD), and depression. We selected these three conditions because they each have high rates of mortality. Depression is associated with high suicide rates. PTSD is also linked to suicide (Krysink and Lester 2010). Individuals with ADHD can put themselves into dangerous situations due to a lack of impulse control, leading to substance abuse, self-injury, contraction of illnesses, and sometimes suicide attempts (Medical News Today, 2015). We selected these three conditions with high mortality to investigate whether the COVID-19 pandemic worsened these symptoms.
COVID-19 has limited the amount of social interactions that are possible. Thus, the pandemic has forced therapy to move online rather than being conducted face-to-face.
There are numerous limitations to online therapy. Many insurance companies do not cover online therapy, which forced many patients to cease their therapy sessions. Body language is also harder for the therapist to deduce via a screen. Patients might not be able to get the most out of their therapy as therapists will have to rely solely on the patient’s facial expressions. Another concern for therapists is technical difficulties that can occur, as they can interfere with therapy sessions, and therapists can come as less empathetic over a video call (Cherry et al., 2020). Although patients’ mental illnesses might worsen during the pandemic, many are not receiving the care they need, leading vulnerable individuals to be hospitalized or even be driven to suicide.
In December of 2021, the CDC reported that deaths due to overdose increased during the pandemic. They recorded the highest number of drug-induced deaths in 12 months. Alcoholism and alcohol-related deaths have also steadily increased. While substance-abuse related deaths might not be caused by the intent to end one’s life, they are still linked to mental illness. This data heavily indicates a need for further research into vulnerable populations in order to develop methods to assist these groups.
Unfortunately, little is known about trends in the worsening of symptoms in ADHD, PTSD, and depression after COVID-19. Therefore, this review will analyze the trends of risk factors for increased symptoms with the hypothesis that different risk factors will be associated with various psychiatric conditions due to their distinct psychological mechanisms.
Methods
During our selection process for the relevant mental health conditions, we focused on ADHD, PTSD, and depression as our team hypothesized that these conditions were likely to worsen during the COVID-19 pandemic due to each condition having a high mortality rate.
In order to find relevant research to include in our analysis, we used the following databases: Google and PubMed. Our search terms were: “COVID’s effect on PTSD”, “COVID-19 and Post Traumatic Stress Disorder”, “COVID-19 and Attention Deficit Hyperactivity Disorder”, “COVID’s effect on ADHD”, “COVID’s effect on depression”, “PTSD worsening and COVID”, “ADHD worsening and COVID”, and “Depression worsening and COVID.” We initially scanned 20 papers before deciding to focus our analysis on 12 papers based on the following inclusion criteria: we only included studies without elderly participants, as we wanted to focus on children and adults, and we did not include studies on participants who had comorbid conditions.
There were several types of bias that may have entered this study. Several co-authors have experienced mental health issues similar to those discussed in the paper, while others have not. This could cause bias due to the fact that some of the co-authors might not identify with their writing while others identify to a certain extent and might add their perspective to the data. To prevent this bias, authors with certain mental conditions did not work on sections of the paper concerning their mental condition. A further bias that might be found in a paper such as this is confirmation bias. Such bias occurs when data is misunderstood or adapted to match a pattern that aligns with previous data. Recall bias and procedural bias both link to the respondents and their truthfulness or accuracy when completing a questionnaire. Recall bias is defined as when participants do not remember past experiences precisely. One way that could impact our results is if subjects did not always remember risk factors for worsening and we would miss risk factors to identify. In contrast, procedural bias is defined as when there is too much pressure on participants so that they finish the survey or questionnaire too quickly. Lastly, publication bias may have entered into this study. Publication bias occurs because journals are more likely to publish studies that found significant differences rather than studies that found no group differences. It is possible that the reason we found significant effects of the pandemic on exacerbation of mental symptoms was publication bias. In fact, patients may have worsened due to natural history of disease or nonoptimal medication management.
We performed a thematic analysis on our selected sources, which included interviews with key opinion leaders, clinical trials, empirical articles, and interviews. Given the novelty of this research, we aimed to find roughly ten sources in total, with at least three sources for each condition.
Results
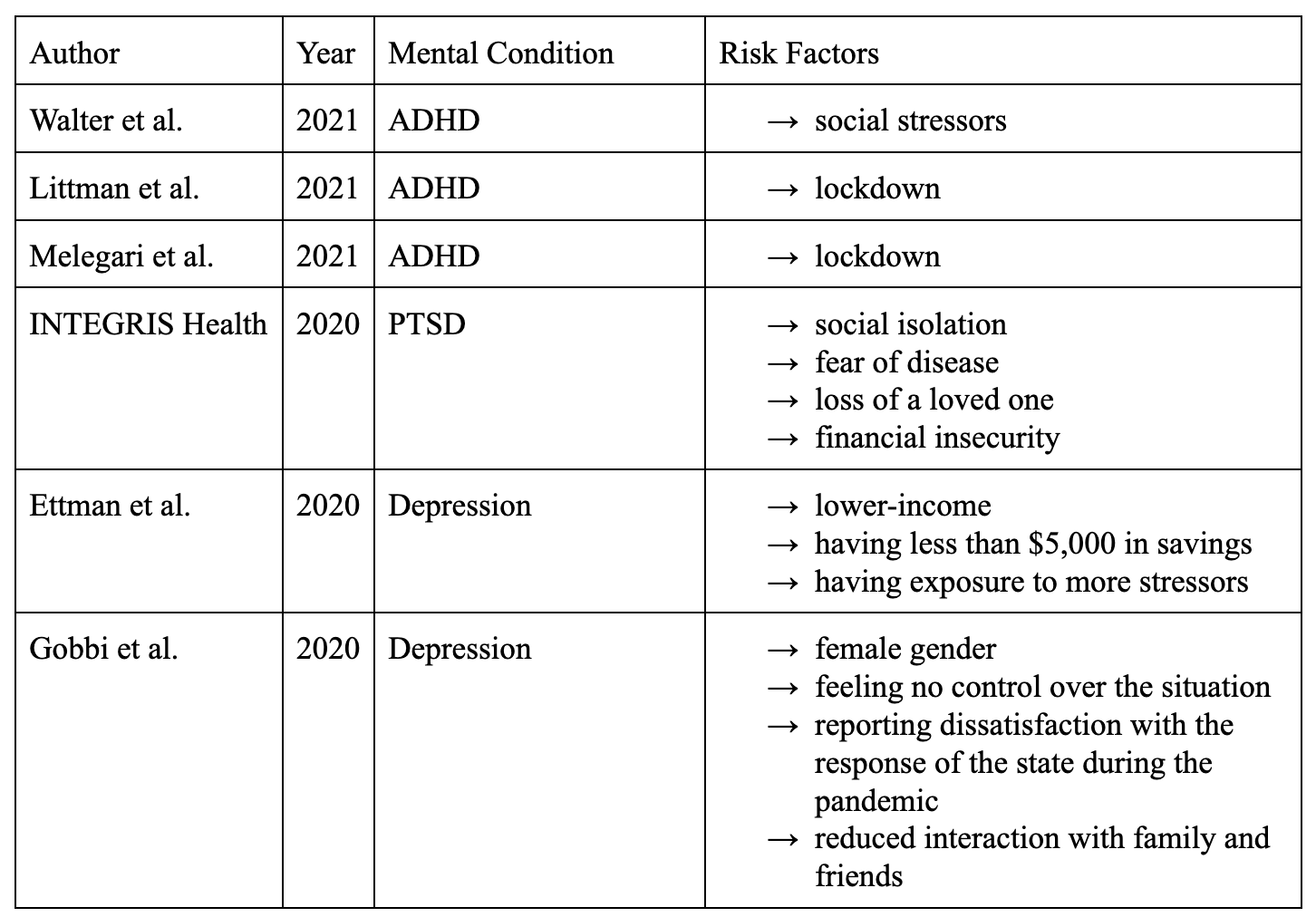
Table 1. Risk Factors for the worsening of ADHD, PTSD, and depression. Articles without risk factors for mental conditions’ symptom worsening are not included in the table.
We collected twelve articles discussing the effects of COVID-19 on ADHD, PTSD, and Depression ranging from 2020 to 2021 (Table 1). There were four sources for each condition.
ADHD
The first of the three conditions we focused on is ADHD. ADHD is one of the most frequent neurodevelopmental disorders of childhood, usually lasting until adulthood.
Many individuals with pre-existing ADHD struggled to complete everyday tasks that are necessary to do, for example, attending online academic or business related calls, having to look after their children, doing regular everyday chores around the house, and any other daily task that would require immense focus. These are just some examples of what ADHD patients would have to endure during the COVID-19 pandemic which made it a difficult time period for patients of all ages.
One study examined the impact of COVID-19 and the lockdown on families caring for children with ADHD (Shah et al., 2021). The study noted an increase in ADHD symptoms including activity level (50.1%), irritability (45.8%), and disturbing or disruptive behavior (47.7%) in children. The viability of carrying out a text message-based intervention was also examined. An online survey was carried out to evaluate the impact of lockdown on children with ADHD and their families. Additionally, a text message based intervention was performed over two weeks. 48 out of the 80 parents from this study initially agreed to participate. 41 agreed to receive an intervention. 29 out of 41 parents filled the satisfaction survey. Text-based messaging was rated on a scale from 0 to 10. It was rated as 5.79 for content, 5.76 for usefulness, and 6 for satisfaction. The key messages of this study are that the lockdown led to the worsening of symptoms in a significant proportion of children with ADHD and that text-based messages for children are a viable intervention.
COVID-19 can irritate symptoms of ADHD, specifically impulsivity. This was made evident by this next study which was an interview with a psychiatrist, David Goodman from the Johns Hopkins School of Medicine focusing on the challenges for adults with ADHD during COVID-19 (Walter, 2021). Impulsivity could lead the individual with ADHD to enter situations in which they are more vulnerable to contracting not only COVID-19 but also other infectious diseases. This is due to the fact patients do not think as much when interacting with others or engaging in high-risk activities. In his conclusion, Goodman says one of the social stresses of the pandemic is that adult ADHD patients with children may have to perform too many tasks between work, home, and the virtual school their children must attend. Goodman also touches on the impact that this pandemic will have on children and students specifically with the task of online learning as that requires the ability to be able to focus on tasks for a prolonged period of time and that can be at times very challenging for a person with ADHD at the best of times, let alone during this pandemic.
Emotional reactivity is defined as the propensity to undergo recurrent and severe emotional arousal. ADHD’s emotional reactivity can create ever-increasing levels of stress due to the pandemic (Littman, 2021). Specifically, ADHD patients virtually report feeling worse with more overwhelming anxiety during COVID-19. Many patients with ADHD felt that lockdown was threatening their stability and their sense of danger triggered a sense of trauma. Prior trauma could consist of the fact that patients with ADHD that had to grow up with parents with ADHD would have experienced living with more impulsive and temperamental parents, and thus would have experienced this feeling of helplessness before. During the COVID-19 pandemic, feelings of helplessness will be highly amplified. Due to the overwhelming sense of distress and danger the virus causes, nothing at home feels necessary to attend to. Therefore, the ADHD brain refuses to complete tasks that need to be done. Self-motivation is difficult to find. Overall, the pandemic triggers trauma responses in the brain for those who have gone through traumatic experiences.
Another study found that subjects who were classified as “low severity degree”, in terms of their mental condition, worsened significantly (Melegari et. al, 2021). However, moderate and severe patients showed important improvement during the lockdown. Patients suffering from symptoms of ADHD such as loss of interest and enjoyment resulting in mood and behavior changes are more strongly affected by the condition of isolation. This was seen in children more frequently. Children and adolescents showed substantially similar trends but children were more prone to emotional fluctuation. The study identifies the impact of the COVID-19 pandemic on the mood and behavior of children, as well as young adults, with ADHD. 992 parents of children and adolescents with ADHD filled out an anonymous online survey through the ADHD Family Association website. The survey studied the degree of severity of 6 states of emotions including sadness, boredom, little enjoyment/interest, irritability, temper tantrums, and anxiety based on a weekly frequency. It also studied 5 disrupted behaviors including verbal and physical aggression, argument, opposition, and restlessness. The study concluded that fluctuations were discovered in all moods and behaviors during the lockdown independently by the severity degree, which corroborates the previous study’s findings of the intensification of symptoms in patients with ADHD from adults to children.
PTSD
Certain events that are associated with the pandemic, such as the loss of a family member or the damaging experiences of being unable to leave the home environment, were shown to exacerbate symptoms in individuals who have PTSD.
One paper concerning PTSD hypothesized that, while the general population might display unwavering strength in the face of the pandemic, the population of those with mental illnesses might experience an exacerbation of their symptoms (INTEGRIS Health, 2020). The paper also showed the effect of gaps in clinical care on the immediate response to COVID-19-related PTSD. This paper examines how COVID-19 can impact or cause PTSD. Distressing experiences through the pandemic such as social isolation, fear of disease, the loss of a loved one, or financial insecurity have caused new cases of PTSD or worsened those already diagnosed.
Another article examines the effects of COVID-19 on specific PTSD symptoms (Brainline, 2021). The authors cite the following five effects:
1) Increased hypervigilance
2) Development of new trauma triggers
3) Inability to do things that are considered safe
4) An increase in intrusive thoughts and feelings
5) Poor sleep and concentration
Depression
The third condition of interest is depression. Individuals with a pre-existing depressive disorder may have experienced an increase in symptoms.
In this study of the prevalence of depression before and after the pandemic, depression symptom prevalence was more than 3-fold higher in the population of those already diagnosed with depression during the COVID-19 pandemic than before (Ettman et al, 2020). Lower income, having less than $5000 in savings and exposure to more stressors were associated with a greater risk of depression symptoms during the pandemic. However, married individuals had lower rates of depression symptoms. This study was a survey on the prevalence of depression symptoms seen in adults. The study question researched the burden of depression symptoms among US adults during the pandemic (before and after), and the risk factors associated with the condition’s symptoms. Depression symptoms in both studies were assessed using the Patient Health Questionnaire–9. The study specifically recruited two different surveys of adults over 18 years old based online, using questionnaires. In this study, many participants did not complete the whole survey. Excluding the incomplete responses, the survey had 1441 respondents from during the COVID-19 pandemic and 5065 respondents from before the coronavirus pandemic. The study hypothesizes that there will be an increase in depression to come, especially in populations at risk of worsening.
The next study exemplified the mental health impact the pandemic had on individuals with and without depressive, anxiety, or obsessive-compulsive disorders (Pan et al., 2021). Although individuals with depressive, anxiety, or obsessive-compulsive disorders scored higher on all four validated symptom scales than individuals without these mental health disorders, both before and during the COVID-19 pandemic, they did not report a greater increase in symptoms during the pandemic. People without depressive, anxiety, or obsessive-compulsive disorders showed a greater increase in symptoms during the COVID-19 pandemic, whereas individuals with the greatest mental health issues tended to show a slight symptom decrease. In three psychiatric case-control cohorts addressed by the study, the authors compared the perceived mental health impact, coping strategies, and changes in depressive symptoms, anxiety, worry, and loneliness before and during the COVID-19 pandemic. The scales used were the 16 item Quick Inventory of Depressive Symptoms (QIDS) for depression, the 21 item Beck Anxiety Inventory (BAI) for anxiety, the 11 item Penn State Worry Questionnaire (PSWQ) for worry, and the six item De Jong Gierveld Loneliness Scale (DJGLS) for loneliness. The comparison was between individuals with and without lifetime depressive, anxiety, or obsessive-compulsive disorders. Online questionnaires were distributed among the Netherlands Study of Depression and Anxiety, Netherlands Study of Depression in Older Persons, and Netherlands Obsessive Compulsive Disorder Association cohorts, including humans with (n=1181) and without (n=336) depressive, anxiety, or obsessive-compulsive disorders. The questionnaire contained questions on perceived mental health impact, fear of COVID-19, coping strategies, and four validated scales assessing depressive symptoms, anxiety, worry, and loneliness used in previous waves during 2006-2016. The number and chronicity of disorders were based on diagnoses in previous waves. The authors summarize that individuals with depressive, anxiety or obsessive-compulsive disorders are experiencing a detrimental impact on their mental health, fear, and coping ability from the COVID-19 pandemic, which requires close monitoring in clinical practice.
In another study, the authors searched the EMBASE, OVID-MEDLINE, and PsycINFO databases to identify potentially eligible studies. Of 1791 records reviewed, fifteen studies were included (Neelam et. al, 2020). Individuals with pre-existing mental illness had significantly higher psychiatric symptoms, anxiety symptoms and depressive symptoms compared to normal controls during a pandemic with pooled effect sizes (SMD) of 0.593 (95% confidence interval (CI) 0.46 to 0.72), 0.616 (95% CI 0.49-0.73) and 0.597 (95% CI 0.38 to 0.80), respectively. This study, a meta-analysis of fifteen studies, investigates the increased symptoms that were caused by the pandemic in those with pre-existing mental illnesses. Studies also found a reduction in psychiatric hospitalizations and utilization of psychiatric services during the pandemic. This review highlights the need for policymakers to plan for an appropriate level of support and care for people with preexisting mental illness during a pandemic. As these patients are scoring higher on these scales, they will be more vulnerable to risk factors during COVID-19.
The final study was aimed at determining the specific factors associated with the worsening of symptoms of psychiatric conditions during the COVID-19 pandemic (Gobbi et al., 2020). The study reported that it received valid responses, mainly from twelve featured countries, indicating a self-reported worsening of psychiatric conditions in two-thirds of patients assessed through their significantly higher scores on scales for general psychological disturbance, post-traumatic stress disorder, and depression. This large study anonymously examined 2734 psychiatric patients worldwide for worsening of their pre-existing psychiatric conditions during the COVID-19 pandemic. An independent clinical investigation of 318 psychiatric patients in the United States was used for verification. Female gender, feeling no control over the situation, reporting dissatisfaction with the response of the government during the COVID-19 pandemic, and reduced interaction with family and friends were associated with increased symptoms of preexisting psychiatric conditions whereas optimism, ability to share concerns with family and friends, and using social media like usual were associated with fewer increases.
In summary, during our research on the subgroup of depression and COVID-19, we found many studies that corroborated the conclusion that the coronavirus intensified the symptoms for many individuals.
Discussion
Of the twelve studies surveyed, most reported a strong pattern of worsening of symptoms in ADHD, PTSD, and depression, respectively, with the exception of one study on ADHD in which the moderate and severe groups showed slight improvement (Melegari et. al, 2021), one study on PTSD that focused on prevalence (Tang et. al, 2020), and one study on depression that showed no change post-pandemic (Pan et al, 2021). A meta-analysis of fifteen studies on depression amongst people with pre-existing mental illness showed significantly higher depressive symptoms compared to normal controls comparing pre-and post-pandemic symptomatology (Neelam et. al, 2020). Of note, in a large study of 992 children and adolescents with ADHD, subjects with a less severe degree of ADHD significantly worsened in six states of emotion and five disrupted behaviors during lockdown (Melegari et. al, 2021). The survey investigated the degree of severity of 6 emotional and mood states (sadness, boredom, little enjoyment/interest, irritability, temper tantrums, anxiety) and 5 disrupted behaviors (verbal and physical aggression, argument, opposition, restlessness) based on their frequency/week (absent; low: 1-2 days/week; moderate: 3-4 days/week; severe: 5-7 days/week) before and during the lockdown. The findings of studies on ADHD concluded that the risk factors that provoked or worsened symptoms associated with ADHD such as impulsivity and irritability were mainly correlated with the stress of managing home-life and a sense of danger.
Of three studies that gave reasoning as to why certain symptoms worsened in some patients but not others, two mentioned high levels of social stress or concerns about the pandemic. Similarly, a large study on PTSD (Shah et al., 2021) concluded that feeling extreme fear was the most significant risk factor for psychological distress followed by short sleep duration. Other risk factors for PTSD symptoms worsening were social isolation, fear of disease, and financial insecurity (INTEGRIS HEALTH et al., 2020). In a large study of over 1000 patients (Shah et al., 2021), the most common risk factors for worsened symptoms found in studies on depression were similarly low-income backgrounds, exposure to more stressors, and lack of social interaction. We can assume that characteristics like financial status could potentially directly influence further worries such as financial insecurity and unemployment in similar conditions. Depression and PTSD were similar in terms of the risk factors of financial factors and social isolation, perhaps because these conditions share similar features such as sleep problems and loss of interest in daily activities, which are not found in ADHD. Whilst PTSD and depression both vary in causes, they are treated similarly through prescribed medication and support groups.
One unexpected finding was that individuals with depression did not record an increase in symptoms during the pandemic, whereas individuals who had not reported experience with depression prior to the pandemic reported a considerable increase in symptoms. This finding was unique to the Netherlands and could be due to population peculiarities or particular healthcare interventions. For example, moderate to severe depression may have been treated more aggressively during the pandemic in the Netherlands, so patients actually get better, whereas those with mild depression may not have accessed medical assistance.
There were other limitations to this study as well. The literature search included interviews of key opinion leaders in addition to peer-reviewed journal articles. We chose to include such sources given the fact that literature on the worsening of symptoms in PTSD, ADHD, and depression during the COVID-19 pandemic is sparse. Of note, we included studies with different age categories, as PTSD, ADHD and depression may affect various age groups differently. We included a wide range of sources with diverse participant demographics in order to gain a more holistic view of a particular disorder. Most importantly, we included studies with various methodologies that may not be directly comparable. An analysis of effects on other psychiatric conditions has yet to be considered.
Future directions for research on this topic include review papers dedicated to each condition. These papers should also include measures of the overall condition worsening, worsening of the condition in key dimensions such as suicidal thoughts, emotional reactivity, new trauma triggers that may cause serious individual debilitation and an analysis of the impact of disease severity groups on differential worsening of symptoms. The magnitude of the risk factors should be examined when possible to inform triaging medical care for ADHD, PTSD, and depression during COVID-19. The impact of telemedicine or other treatment differences on worsening each condition should also be considered.
It is paramount for optimization of mental healthcare delivery (e.g. telemedicine and suicide prevention helplines) during these challenging times that the most vulnerable populations and risk factors be efficiently identified.
Conclusion
Overall, there was a worsening of symptoms in ADHD, PTSD, and depression during the COVID-19 pandemic. The risk factors identified for the individual subgroups were different given their different symptoms and conditions. For ADHD, risk factors included the stress of controlling life at home and feeling unsafe and/or fearful. PTSD mainly included the fear of losing loved ones, catching the virus, shorter sleep duration, social isolation, fear of disease, and financial insecurity. The most common risk factors for worsened symptoms in depression were a low-income background, feeling a lack of control, lack of social interaction, and dissatisfaction with the response of the state during the pandemic. Isolation was a risk factor for all of these conditions.
Future directions for research on PTSD, ADHD, and depression include meta-analyses dedicated to each condition, examination of the magnitude of risk factors, and the development of methods to help improve individualized medical care.
Bibliography
ADHD “doubles the risk of early death”. (2015, February, 26 ). Medical News Today. https://www.medicalnewstoday.com/articles/289931#1
Cherry, K. (2020, September 20). The Pros and Cons of Online Therapy (S. Gans, Ed.). https://www.verywellmind.com/advantages-and-disadvantages-of-online-therapy-2795225
Cullen, W., Gulati, G., & Kelly, B. D. (2020, March 30). Mental health in the Covid-19 pandemic. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7184387/
Effects of the Coronavirus (COVID-19) Pandemic on PTSD. (2021, June 7). BrainLine. https://www.brainline.org/article/effects-coronavirus-covid-19-pandemic-ptsd
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open. 2020 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2770146
INTEGRIS Health. (2020, June 22). How the Coronavirus May Impact or Cause PTSD. https://integrisok.com/resources/on-your-health/2020/june/ptsd-and-coronavirus
Gobbi, S., Płomecka, M. B., Ashraf, Z., Radziński, P., Neckels, R., Lazzeri, S., Dedić, A., Bakalović, A., Hrustić, L., Skórko, B., Es Haghi, S., Almazidou, K., Rodríguez-Pino, L., Alp, A. B., Jabeen, H., Waller, V., Shibli, D., Behnam, M. A., Arshad, A. H., . . . Jawaid, A. (2020). Worsening of Preexisting Psychiatric Conditions During the COVID-19 Pandemic. Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.581426
Krysinka, K., & Lester, D. (2010, January 27). Post-Traumatic Stress Disorder and Suicide Risk: A Systematic Review. https://www.tandfonline.com/doi/full/10.1080/13811110903478997
Littman, E., PhD. (2021, March 24). How This Pandemic Triggers Trauma Responses in the ADHD Brain. ADDitude. https://www.additudemag.com/trauma-coronavirus-adhd/
Melegari, M. G., Giallonardo, M., Sacco, R., Marcucci, L., Orecchio, S., & Bruni, O. (2021). Identifying the impact of the confinement of Covid-19 on emotional-mood and behavioural dimensions in children and adolescents with attention deficit hyperactivity disorder (ADHD). Psychiatry research, 296, 113692. https://doi.org/10.1016/j.psychres.2020.113692
Moore, R. C., Depp, C. A., Harvey, P. D., & Pinkham, A. E. (2020, May 22). Assessing the Real-Time Mental Health Challenges of COVID-19 in Individuals With Serious Mental Illnesses: Protocol for a Quantitative Study. JMIR Publications. https://www.researchprotocols.org/2020/5/e19203#ref1
Neelam, K., Duddu, V., Anyim, N., Neelam, J., & Lewis, S. (2021). Pandemics and pre-existing mental illness: A systematic review and meta-analysis. Brain, behavior, & immunity – health, 10, 100177. https://doi.org/10.1016/j.bbih.2020.100177
Pan, K. Y., Kok, A., Eikelenboom, M., Horsfall, M., Jörg, F., Luteijn, R. A., Rhebergen, D., Oppen, P. V., Giltay, E. J., & Penninx, B. (2021). The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. The lancet. Psychiatry, 8(2), 121–129. https://doi.org/10.1016/S2215-0366(20)30491-0
Quadir, S. (2021, April 27). People with mental illnesses report worsening symptoms during lockdown. City, University of London. https://www.city.ac.uk/news-and-events/news/2021/04/people-mental-illnesses-report-worsening-symptoms-lockdown
Shah, R., Raju, V. V., Sharma, A., & Grover, S. (2021). Impact of COVID-19 and Lockdown on Children with ADHD and Their Families-An Online Survey and a Continuity Care Model. Journal of neurosciences in rural practice, 12(1), 71–79. https://doi.org/10.1055/s-0040-1718645
Walter, K. (2021, January 15). David W. Goodman, MD: Adult ADHD Challenges During COVID-19. HCPLive. https://www.hcplive.com/view/goodman-adult-adhd-challenges-covid-19
Yao, H., Chen, J.-H., & Xu, Y.-F. (2020, April 7). Patients with mental health disorders in the COVID-19 epidemic. https://pubmed.ncbi.nlm.nih.gov/32199510/




