Abstract
This research paper aims to discuss and explore lung cancer during pregnancy for non-smokers. Cases of gestational lung cancer have increased over the last decade (Zhou et al., 2023). It is important to understand risk factors, treatment options, and the increased severity of lung cancer during pregnancy compared to non-gestational lung cancer as it improves decision-making skills and outcomes, allows for more tailored medical care, and supports education, research and medical advancements (Zhou et al. 2023).
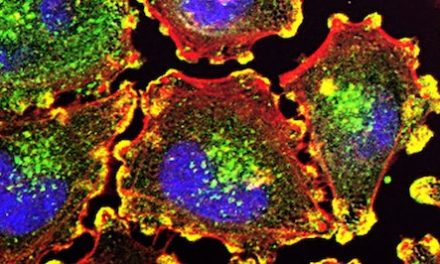
Prevalent in non-smokers, lung cancer can occur through metastasis, commonly known as metastatic lung cancer. This happens when cancerous cells from primary tumors travel through the bloodstream and lymph nodes, forming secondary tumors at new sites. According to BioMed Central (BMC Cancer), Metastatic Lung Cancer is ubiquitous (present, appearing, or found everywhere) and approximately 50% of lung cancer cases occur as a result of metastasis (Niu et al., 2016).
Introduction
Overview of Lung Cancer during Pregnancy
Historically, lung cancer is more prevalent in men, however, lung cancer is becoming more prevalent in women, especially in pregnant women. According to the National Library of Medicine, lung cancer is more severe/advanced during pregnancy (Zhou et al., 2023). More commonly found in the placental and fetal metastasis, one of the risk factors of lung cancer during pregnancy is an increase in maternal age at the time of conception (Zhou et. al., 2023) Lung cancer in pregnant women can also cause birth defects and other major problems for the fetus.
Lung cancer is best treated when found early, before or during pregnancy. Lung cancer may show symptoms, for example of a cough or chest pain, and therefore can often be misdiagnosed as pneumonia, affecting both the fetus and the mother during pregnancy and postpartum. The impact of lung cancer on both the mother and fetus varies significantly depending on the timing and type of treatment. Chemotherapy, a form of treatment necessary for managing the disease, can lead to adverse outcomes based on the trimester in which it is given. For example, according to multiple studies, chemotherapy has been associated with an increased chance of miscarriage, especially when given in the first trimester (OTIS, 2023). Fetuses exposed to maternal cancer treatments can experience developmental and cognitive impairments, birth defects, preterm delivery, and low birth weight, however individual developmental outcomes can vary widely (OTIS, 2023). Despite the rising incidence of lung cancer among women, it remains rare during pregnancy, with only 93 reported cases in the literature from 1953-2022 (Zhou et al., 2023). This article explores the clinical characteristics, outcomes, and treatment strategies for lung cancer in pregnant women through literary findings emphasizing the cause in non-smokers.
While smoking is a well-known risk factor for lung cancer, a significant portion of cases occur in non-smokers. Among the 93 documented instances of lung cancer during pregnancy from 1953 to 2022, 28.4% were non-smokers, underscoring the need to investigate other contributing factors, such as genetic predispositions and environmental exposures (Zhou et al. 2023). Regarding non-smoker patients with lung cancer, it becomes more difficult to determine the main risk factors and what can be done in the prevention of the disease.
Demographics of Lung Cancer In Women: During Pregnancy for Non-Smokers
The first cases of lung cancer during pregnancy were recorded in 1953 (Mitrou et al., 2015). Between 1953-2022, there were 93 databases recorded and published instances of lung cancer in pregnant women, with an average age of 34 (Zhou et al., 2023). From 1953-2015, there were a total of 66 confirmed cases of lung cancer in pregnant women (Mitrou et al., 2015), indicating that during the 7 years from 2015-2022, there were 27 further confirmed cases – a little under a third of the total cases recorded up to 2022.
There is an upward trend in the diagnosis of lung cancer in pregnant women: 82.8% of the total cases (93) up to 2022 were recorded after 2000. 12.9% of these 93 women were diagnosed with small cell lung cancer (SCLC), while 87.1% were diagnosed with non-small lung cancer (NSCLC) (Zhou et al., 2023). Within that percentage of women diagnosed with NSCLC (81 women), adenocarcinoma was diagnosed in 56 women, 10 with squamous cell carcinoma, 8 chronic lymphoma leukemia, and 7 other subtypes of NSCLC (Zhou et al., 2023). It should be noted that 27% of women were classified as smokers, 48.4% of these women were classified as nonsmokers, and 23.7% were classified as unknown, according to the Women’s Health Reports narrative review done by Jian Ping Zhou and others (Zhou et al., 2023).
An early diagnosis of lung cancer in women during pregnancy is crucial to ensuring a healthy and safe pregnancy for the fetus and the mother; 8 of the 93 women (1953-2022) were diagnosed before pregnancy, 78 were diagnosed during pregnancy (median gestational week of 26 weeks), and 7 after they delivered the baby (with a median week of delivery of 33 weeks of pregnancy) (Zhou et al., 2023). The TNM stage (description of cancer referring to its size and how far it has metastasized) demographics are 3.2% in 1-2, 8.6% in 3, 83.9% in 4, and 4.3% unknown (Zhou et al., 2023).
Effects on Mother and Baby
The rates of lung cancer during pregnancy have been growing rapidly over the past two decades. Treatments including chemotherapy often lead to birth defects for the baby, and can have short-term or long-term effects on both neonate and mother. Exposure to chemotherapy during the first trimester of pregnancy increases the chances of birth defects above the background risk (OTIS, 2023), and is less likely to cause birth defects when administered in the second or third trimester than during the first (OTIS, 2023). Extensive medical evidence indicates that certain chemotherapeutic agents are more strongly associated with an increased risk of birth defects compared to others (Shenoy et al., 2014). This finding is particularly critical, as the brain and reproductive system continue to be highly sensitive to these medications even after the first trimester of pregnancy, potentially impacting long-term developmental outcomes such as cognitive function, neurological health, and fertility. It is important to consider how the number of medications used during pregnancy, how often they’re taken, how long the medications are used for, and the trimester in which they are used, all affect the baby’s health (OTIS, 2023). The risks of preterm delivery, stillbirth, low birth weight, admission to the neonatal intensive care unit, and a transient decrease in some of the baby’s blood cells have all been linked to exposure to chemotherapeutic medications during the second and third trimesters (OTIS, 2023).
Preventative Measures of Lung Cancer
Several preventive measures can be taken to reduce the risk of developing lung cancer. These measures include abstaining from tobacco use, minimizing exposure to radon and other cancer-causing agents, and refraining from household coal combustion (National Cancer Institute, 2024). Furthermore, inhalation of naturally occurring asbestos minerals, commonly used in various building materials and industrial settings, has been linked to an increased susceptibility to lung cancer (National Cancer Institute, 2024). Occupations associated with the highest risk of asbestos exposure include workers in asbestos mines, automotive industry employees (including brake and clutch repair workers), shipyard workers, cement plant employees, plumbing and heating tradespeople, construction workers, painters, carpenters, and electricians. OSHA recommends that individuals working in environments with potential asbestos exposure wear protective clothing made of synthetic fabrics specifically designed to block tiny asbestos fibers (Occupational Safety and Health Administration, 2024). This may include synthetic coveralls, respiratory masks, boots, and gloves.
Additionally, the inhalation of silica dust poses a grave risk to respiratory health due to its minute size, which is about 100 times smaller than a grain of sand, allowing for undetected inhalation. Exposure to silica dust can have serious health implications, including the onset of lung cancer, irreversible lung scarring, kidney disease, and chronic obstructive pulmonary disease. It is estimated that approximately 230 individuals annually develop lung cancer due to past exposure to silica dust in their workplaces (Cancer Council, 2019). It is important to note that not all individuals exposed to silica dust will develop cancer; however, the likelihood of cancer incidence rises with prolonged or repeated exposure to high levels.
The Need for Special Attention
Treatment Options for Lung Cancer During Pregnancy
The treatment of lung cancer during and after pregnancy involves a careful balance: it is essential to ensure the effectiveness of cancer therapies and the minimisation of risks to both the mother and the fetus. Postpartum treatment offers more flexibility and has proven more effective with targeted therapies, whereas treatment during pregnancy requires tailored approaches including safe surgical interventions, advanced imaging techniques, and genomic profiling to guide therapy (Smith et al., 2015). After delivery, postpartum treatment for lung cancer in women includes a range of therapies tailored to the cancer’s type and stage. Interestingly, a recent study showed no evidence of congenital malformations in patients who received chemotherapy (docetaxel, gemcitabine, and cisplatin) during the first trimester (National Library of Medicine, 2024). Platinum-based chemotherapy, often combined with targeted therapies such as tyrosine kinase inhibitors (TKIs), is a common approach (Smith et al., 2015). According to a comprehensive review of cases from 1953-2015, patients treated postpartum with these targeted therapies have experienced extended survival rates without significant adverse effects on their health (Johnson et al., 2018). However, waiting until postpartum to treat lung cancer poses significant risks, including the potential for cancer progression to a more advanced stage, which can reduce overall survival rates for the mother. The delay in treatment can allow the cancer to spread, making it more challenging to manage and decreasing the likelihood of a successful outcome.
While targeted therapies like TKIs have shown effectiveness for certain lung cancer biomarkers, their safety during pregnancy remains uncertain due to limited evidence. Studies have suggested potential risks to the fetus and the lack of comprehensive data warrants caution when considering these therapies for pregnant patients (Johnson et al., 2018). Surgical intervention can be a viable treatment option for lung cancer during pregnancy. Surgery, particularly intra-abdominal surgery, is ideally performed in the early second trimester to minimise risks to both the mother and the fetus (Lee et al., 2020). The timing of the surgery is crucial to avoid complications associated with early pregnancy and the physiological changes that occur later on during pregnancy. Tumor genomic profiling has become an essential component of lung cancer management, even during pregnancy. This approach helps identify specific genetic mutations that can help guide targeted therapy decisions (Brown et al., 2019). Profiling is especially important for younger patients and those who have never smoked as they may possess unique genetic markers that influence treatment options. Ultrasound and Whole-Body Diffusion-Weighted Magnetic Resonance Imaging (MRI) are crucial for diagnosing and monitoring lung cancer during pregnancy without exposing the fetus to harmful radiation (Miller et al., 2017). Whole-body diffusion-weighted MRI, offers particularly detailed images of cancer that has spread and can be safely used throughout pregnancy.
A surgical biopsy is a necessary step to obtain a definitive diagnosis and to guide treatment planning. When possible, it is preferable to delay this procedure until the second or third trimester to reduce risks associated with anesthesia and surgical stress during early pregnancy. Conducting a surgical biopsy during the first trimester poses several risks, including the potentially teratogenic effects of anesthetic agents, increased risk of miscarriage, and adverse effects on fetal development due to surgical stress and maternal physiological changes. During the second and third trimesters, the risks are comparatively lower as the fetus is more developed and the critical period of organogenesis has passed. However, careful consideration must still be given to the type of anesthesia used and the surgical technique to minimize any potential harm to both the mother and the fetus. The decision to perform a surgical biopsy must be made collaboratively by a multidisciplinary team, taking into account the urgency of the diagnosis and the overall health of the mother and the fetus (Davis et al., 2021).
Psychological Impact of Lung Cancer Diagnosis During Pregnancy
The psychological impact of a lung cancer diagnosis during pregnancy is profound, affecting both the mother and the developing child (Zhou et al., 2023). For mothers, the diagnosis can trigger a range of emotional responses, including anxiety, depression, and a sense of helplessness. These feelings are often exacerbated by the stress of managing a complex medical condition while also preparing for the arrival of a new baby (Rubens et al., 2020). In a recent study by Betchen et al., mothers diagnosed with cancer during pregnancy often experience significant psychosocial distress, which can impede their ability to bond with their newborn and participate in early childcare activities (Betchen et al., 2020). Concerns about the potential impact of cancer treatments on fetal development further intensify this psychological strain.
Children born to mothers with cancer during pregnancy may face unique developmental challenges. A study by Cardonick and colleagues compared in-utero chemotherapy-exposed children with non-exposed controls and found no significant differences in cognitive development and behaviour (Cardonick et al., 2015). However, the study did highlight the potential for increased maternal anxiety to indirectly influence child development. Elevated maternal stress levels during pregnancy have been associated with adverse outcomes in children, including lower birth weights and preterm deliveries, which can, in turn, affect cognitive and physical development (Rubens et al., 2020).
The experience of undergoing cancer treatment during pregnancy can have long-lasting effects on maternal mental health. Betchen et al reported that mothers who received a cancer diagnosis while pregnant often continue to struggle with psychological issues long after the treatment has concluded. The dual responsibilities of managing their health and caring for their child can lead to chronic stress and emotional exhaustion. This ongoing stress can impair maternal functioning, leading to difficulties in parenting and negatively impacting the child’s emotional well-being and development (Mitrou et al., 2015).
For non-smoking mothers, the psychological burden may be compounded by confusion and frustration over the diagnosis, as they often face additional stress due to the stigma associated with lung cancer. Non-smokers may struggle to understand how they developed the disease despite not engaging in common risk behaviours, leading to a heightened sense of vulnerability and fear regarding their prognosis and the future of their child. Addressing these psychological impacts requires a comprehensive approach, including targeted psychological support and counselling, to help mothers cope with their diagnosis, manage treatment-related stress, and to foster a healthy developmental environment for their children (Zhou et al., 2023).
The psychological impact of a lung cancer diagnosis during pregnancy on mothers and their children is multifaceted and significant. It necessitates a multidisciplinary approach to care that addresses both the physical and emotional needs of the mother and provides support to optimise child development outcomes. This comprehensive care strategy can help mitigate the adverse effects of the diagnosis and treatment, promoting better long-term health and well-being for both the mother and the child.
The Genetic Risk of Non-Smokers
Although smoking history is one of the main risk factors for lung cancer (including lung cancer during pregnancy), tobacco is not the only factor contributing to lung cancer in women; according to Sotirios Mitrou and others in the Journal of Advanced Research, under 50% of patients have a positive smoking history. The study also suggests that the estimated glomerular filtration rate (eGFR) and anaplastic lymphoma kinase (ALK) have implications on the genetic risk of non-smokers.
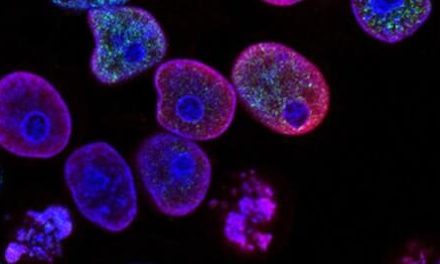
The epidermal growth factor receptor (EGFR) mutation is a very common genetic mutation present in non-small cell lung cancer patients; EGFR is a protein on the surface of somatic cells (most commonly found in skin cells) that allows them to grow. Since cancer is the uncontrollable growth of cells, an EGFR genetic mutation can cause a cell to grow more than it should, causing cancer. The most common type of EGFR mutation is an EGFR L858R point mutation, where the DNA is misspelled when a single nucleotide is changed, or an EGFR 19 deletion (DNA missing sequences), but the mutation could also be an insertion (additional codons added to DNA) or another type of deletion in the DNA (Haghighi, 2023). Most often, EGFR-positive lung cancer is expressed as adenocarcinoma.
ALK-positive lung cancer is heavily associated with lung cancer in non-smokers. The correlation between ALK-positive lung cancer and outside factors such as environmental toxins (such as first- or second-hand smoking, asbestos, or air pollution) is unknown. This type of genetic mutation is caused by a rearrangement of the ALK gene found on chromosome 2; however, it is unknown why the rearrangement happens (Lindeman et al., 2018). The ALK gene is responsible for the assembly of the ALK receptor tyrosine kinase protein, a protein that transmits signals from the cell surface into the cell through signal transduction (MedlinePlus Bethesda, 2011). Mutated forms of the gene are often expressed as neuroblastoma, non-small cell lung cancer, and anaplastic large cell lymphoma. The most common mutation in neuroblastoma is the replacement of the amino acid arginine with glutamine at position Arg1275Gln/R1275Q (MedlinePlus Bethesda, 2011). If an ALK receptor tyrosine kinase is mutated or overexpressed, it will no longer require external stimulation to be phosphorylated. Thus, the kinase and signaling pathway (downstream) are constitutively activated, which may increase the growth of immature nerve cells, ultimately leading to neuroblastoma (MedlinePlus Bethesda, 2011).
Additionally, according to the Women’s Health Report, it has been reported that an extended fertility span and delayed onset of menopause are linked to lung adenocarcinoma (ADC) (Zhou et al., 2023). Lung adenocarcinoma, the most prevalent form of primary lung cancer in the United States, is categorised as a type of non-small cell lung cancer (NSCLC) and exhibits a significant correlation with prior tobacco use (Myers and Wallen, 2023).
Being aware of the genetic risk of lung cancer in pregnant patients is crucial as it can have a significant impact on both the mother and the unborn child. Understanding the genetic predisposition to lung cancer can aid in making well-informed decisions about treatment options and in providing the necessary support and care for the patient. This knowledge can also help in assessing the potential risks to the fetus and in developing a tailored healthcare plan that considers the specific needs and challenges associated with both pregnancy and cancer treatment.
Doctor Appointments/Additional Meetings
Pregnant women diagnosed with lung cancer often have frequent pediatric meetings for the fetus and doctor visits to monitor the spread/stability of the cancer. Frequent meetings with doctors and oncologists are important. It is very important to know all the information that you can to help provide enough resources to get pregnant mothers to have a safe delivery. According to the American Cancer Society, imaging appointments might be needed but the main concern with imaging is what might happen to the fetus (American Cancer Society, 2022). Having an X-ray during pregnancy is considered high risk as exposure to radiation could be potentially fatal for the fetus. To fully understand all the risks that cancer might carry throughout one’s pregnancy, it is crucial that frequent doctor appointments and meetings occur. This allows for safe options for both the baby and the mother.
The Need to Increase Awareness of Lung Cancer During Pregnancy
Case Study: An Illustrative Example
Here we review a case study of a pregnant patient with lung cancer to illustrate the unique challenges and considerations in this sensitive situation in order to highlight the importance of personalised care during pregnancy. The case described pertains to a 26-year-old African-American female non-smoker who received a diagnosis of Stage IIIA squamous cell carcinoma of the lung with lymphoepithelioma-like features (large, syncytial cells) during the 18th week of her pregnancy (Yates and Zhang, 2015).
After a chest CT scan, a substantial right hilar mass obstructing the right main bronchus, the collapse of the right lung, and subsequent mediastinal shift to the right were all observed (Yates and Zhang, 2015). Confirmation of poorly differentiated squamous cell carcinoma with lymphoepithelioma-like features was obtained through a transbronchial biopsy and subcarinal lymph node analysis (Yates and Zhang, 2015). Further diagnostic evaluations, including brain MRI, PET, and CT scans, revealed no indication of distant metastasis (Yates and Zhang, 2015).
The patient underwent four cycles of neoadjuvant cisplatin and docetaxel (chemotherapy medications), resulting in a complete radiographic response (Yates and Zhang, 2015). Subsequently, she successfully delivered a healthy baby girl at 35 weeks of development (Yates and Zhang, 2015). Post-partum, the patient received radiation to the right hilum and mediastinum for consolidation (Yates and Zhang, 2015). Notably, the patient remains free of disease more than 16 months after the initial diagnosis (Yates and Zhang, 2015). To the best of our knowledge, this case represents the sole reported instance of lung cancer during pregnancy with a complete response to chemotherapy. While this case demonstrates a positive outcome, it is important to note that further research and data are required to make general conclusions about the effectiveness of chemotherapy during pregnancy. Thus, it is imperative to conduct additional studies to establish the best possible treatment strategies for pregnant women facing similar conditions.
Global Impact
To raise awareness of lung cancer in pregnant patients, it is imperative to utilise various modes of communication to ensure that awareness is raised among both healthcare professionals and the general public. By collaborating with obstetricians, oncologists, and other healthcare providers, targeted educational materials and resources can be developed. The focus of this public health messaging should be on the distinctive challenges and considerations surrounding the management of lung cancer in pregnant women, including the potential impact of different treatment options on fetal development, the ethical considerations of balancing the mother’s health with the well-being of the fetus, and the multidisciplinary approach involving various specialists.
Additionally, organising educational seminars and webinars specifically tailored to healthcare professionals can help circulate essential information about identifying and managing lung cancer in pregnant patients. These events can also provide a platform for discussing available guidelines and best practices for tailored approaches to care in this specific population. Furthermore, reaching out to the public through social media campaigns, informational websites, and community events can help raise awareness among pregnant women and their support networks. Sharing real-life stories of women who have navigated lung cancer treatment during pregnancy can provide valuable insight and emotional support, while also spreading awareness about the importance of early detection and appropriate management.
Thanks to additional awareness and knowledge surrounding the rise of lung cancer during pregnancy in nonsmokers, a routine lung cancer health check can be mandated for pregnant patients during their early visitations. This proactive approach aims to catch the cancer early if it is present, offering better treatment outcomes and safeguarding the health of both the mother and the unborn child. By implementing these strategies, we can move towards a future where lung cancer in pregnancy is detected early and managed effectively, ensuring healthier outcomes for families worldwide.
By developing targeted educational materials, collaborating with healthcare professionals, and engaging with the public through various channels, we can effectively raise awareness of lung cancer in pregnant women and promote early intervention and support.
Conclusion
This research paper aimed to explore the complexities of lung cancer during pregnancy for non-smokers, a relatively rare clinical scenario that is growing in prevalence each year. Healthcare providers must balance the treatments to help the health of the mother with lung cancer and the development of the growing fetus, as cancer treatments are often harmful. Lung cancer in non-smokers poses particular challenges: these patients are often present with advanced and aggressive disease stages. The non-specific symptoms, which mimic less serious conditions such as pneumonia, can lead to misdiagnosis and delayed treatment, exacerbating the risks for both mother and fetus. Early detection is crucial for improving outcomes, yet the rarity of the condition means it is often not considered until the disease has progressed. As mentioned previously, the median week of diagnosis is at the 26th week of gestation, with a high proportion presenting at stage IV. This late-stage diagnosis underscores the importance of increased vigilance when screening for lung cancer in pregnant women, especially non-smokers who may not be considered high risk.
Bibliography
Gil, S., Goetgheluck, J., Paci, A., Broutin, S., Friard., Couderc, L.J., et al. (2014). Efficacy and safety of gefitinib during pregnancy: a case report and literature review. Case Reports, 85(3). https://doi.org/10.1016/j.lungcan.2014.06.003
Mitrou, S., Petrakis D., Fotopoulos G., Zarkavelis G., and Pavlidis N. (2015). Lung cancer during pregnancy: A narrative review. Journal of Advanced Research. National Library of Medicine, 7(4). 10.1016/j.jare.2015.12.004
Myers, D., Wallen M. Jason (2023). Lung Adenocarcinoma, StatPearls. National Library of Medicine.
National Cancer Institute (2024). Lung Cancer Prevention (PDQ®)–Patient Version. Available at: https://www.cancer.gov/types/lung/patient/lung-prevention-pdq (Accessed: 21 June, 2024).
Niu, F.Y., Zhou, Q., Yang, J.Y., Zhong, W.Z., Chen, Z.H., Deng, W., et al. (2016). Distribution and prognosis of uncommon metastases from non-small cell lung cancer, BMC Cancer, 16. 10.1186/s12885-016-2169-5
Yates, R., Zhang, J. (2015). Lung Cancer in Pregnancy: An Unusual Case of Complete Response to Chemotherapy, Cureus. National Library of Medicine, 7(12). 10.7759/cureus.440
Zhou, J.P., Wang, Y., Lin, Y.N., Sun, X.W., Ding, Y.J., Yan, Y.R., et al. (2023). Clinical Features and Management of Lung Cancer During Pregnancy: A Narrative Review Based on Reported Cases, Women’s Health Report. National Library of Medicine, 4(1). 10.1089/whr.2023.0085
(2022). Cancer During Pregnancy, American Cancer Society. https://www.cancer.org/cancer/managing-cancer/making-treatment-decisions/cancer-during-pregnancy.html
(2011). ALK Gene, Medline Plus. National Library of Medicine. Accessed at: https://medlineplus.gov/genetics/gene/alk/#conditions
Lindeman N.L., Cagle, P., Aisner, D., Arcila, M., Beasley, M., Bernicker, E., et al. (2018). Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors: Guideline From the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology, Archives of Pathology & Laboratory Medicine, 142(3). https://doi.org/10.5858/arpa.2017-0388-CP
What is ALK-Positive Lung Cancer, ALK Positive. Accessed at: https://www.alkpositive.org/what-is-alk#:~:text=ALK%2Dpositive%20lung%20cancer%20is%20caused%20by%20a%20rearrangement%20of,know%20why%20this%20rearrangement%20happens.&text=Lung%20Cancer%20is%20the%20most,patients%20are%20diagnosed%20ALK%2Dpositive.
Haghighi A.S., et al., (2023). What is EDGR-positive lung cancer?, Medical News Today. Accessed at: https://www.medicalnewstoday.com/articles/egfr-mutation-lung-cancer.
(2024) “EGFR and Lung Cancer,” American Lung Association. Accessed at: https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/symptoms-diagnosis/biomarker-testing/egfr#:~:text=EGFR%20(epidermal%20growth%20factor%20receptor,different%20types%20of%20EGFR%20mutations .
Tseng C.H., Chiang, C.J., Tseng, J.S., Yang, T.Y. Hsu, K.H., Chen, K.H., et al., (2017). EGFR mutation, smoking, and gender in advanced lung adenocarcinoma, Oncotarget. National Library of Medicine, 8(58). 10.18632/oncotarget.21842
Siew-Fei N., Ngan, H. (2015). Chemotherapy during pregnancy, Best Practice & Research Clinical Obstetrics & Gynaecology. National Library of Medicine, 28(8). 10.1016/j.bpobgyn.2015.10.007
Rubens, M., Ramamoorthy, V., Saxena, A., McGranaghan, P., Appunni, S., Ahmed, M.A., et al. (2020). Maternal and fetal outcomes of cancer treatment during pregnancy, Clinical Cancer Research. National Library of Medicine, 26(8). 10.1038/s41598-022-13852-4
Tseng C.H., et al. (2022). Chemotherapy exposure in pregnancy, National Center for Biotechnology Information. [NCBI Bookshelf](https://www.ncbi.nlm.nih.gov/books/NBK582629/#:~:text=Exposure%20to%20chemotherapy%20early%20in,the%20first%20trimester%20of%20pregnancy).