Introduction
Post-traumatic stress disorder (PTSD) is a mental condition that occurs in individuals who have experienced traumatic events, such as accidents, war, sexual assault, abuse, and life-threatening situations (Yehuda et al., 2015; National Institute of Mental Health, 2023). Symptoms of PTSD include intrusive flashbacks, poor concentration, sleep disturbances, hypervigilance, avoidance of traumatic stimuli and personal emotions, irritability, strained relationships, dissociation, negative self-image and worldview, self-destructive behaviours, and general estrangement from others as well as reality (Yehuda et al., 2015; Schrader and Ross, 2021).
The U.S. Department of Veteran Affairs estimates that approximately 6% of people in the world will experience PTSD at least once in their lifetime, with women having a higher chance of developing the disorder than men (National Institute of Mental health, 2023). Meanwhile, for UK citizens the probability of having PTSD is 8.9% (McManus et al., 2009). Many other conditions may also increase the risk of getting PTSD, such as Autistic Spectrum Disorder (ASD). A study showed that approximately 40% of adults with ASD displayed intense PTSD symptoms one month before the study and 60% of adults with ASD reported probable PTSD throughout their lifetime (Rumball et al., 2020). Another study researched the frequency of different traumatic scenarios as a cause for PTSD. The results demonstrated almost 42.7% of individuals with PTSD developed it due to sexual violence of any sort, with 13.1% accounted for rape, 15.1% for other sexual assaults, and 9.8% for stalking. Another relatively common cause for PTSD was the unexpected death of a loved one, which accounted for 11.6% of PTSD cases. The article states that sexual violence, though less common than the death of someone close, is a trauma with high PTSD development risk (Kessler et al., 2017).
With years of research, trauma-focused psychotherapies such as Cognitive Processing Therapy (CPT), Prolonged Exposure Therapy (PE), and Eye Movement Desensitization and Restructuring (EMDR), proved to be the most efficacious in treating individuals suffering from PTSD (Yehuda et al., 2015; Schrader and Ross, 2021). Results also showed that patients who undergo therapy experience a greater long-term resolution of symptoms than those who utilise pharmaceuticals. However, selective serotonin reuptake inhibitors (SSRIs) and serotonin noradrenaline reuptake inhibitors (SRNIs) have produced significant results in PTSD treatment. More research is currently being performed on the treatment of PTSD (Yehuda et al., 2015; Hoskins et al., 2021).
There are three different brain regions that are involved and affected in the development of PTSD. These brain regions include the hippocampus, the amygdala, and the medial frontal cortex (Bremner, 2006). Brain scans performed on those suffering from PTSD have revealed that the amygdala, which is in charge of hypervigilance, shows increased activity; the hippocampus, which controls stress responses, has a reduced volume and activity; the prefrontal cortex has a reduced volume, which causes an imbalance of executive functions; the anterior cingulate has reduced volume, which damages the activation of fear responses; and there is a decreased activity of the medial prefrontal cortex, although its effects are yet to be understood (Sherin and Nemeroff, 2022). In recent years there have been several discussions on whether the volume of the hippocampus shrinks with exposure to trauma. However, this is a question that is yet to be answered (Sherin and Nemeroff, 2022).
Origin of PTSD in Different Demographics
The Different Effects of PTSD on Women, Men and Children, and Their Responses
People with PTSD may display various different symptoms depending on the gender and age of the person exposed to a traumatic event. Post-traumatic stress disorder significantly impacts women, leading to unique psychological and emotional responses following traumatic experiences. Research indicates that women are disproportionately affected by PTSD, with prevalence rates estimated between 10-12% for women, compared to 5-6% for men (Breslau et al., 2022). The types of trauma that women typically encounter, such as sexual assault, domestic violence, and childhood abuse, contribute to a distinct symptom profile characterised by heightened anxiety, depression, and interpersonal difficulties (Friedman et al., 2021).
Women with PTSD experience a range of symptoms that can be broadly categorised into emotional, physical, and behavioural manifestations. Emotionally, they often struggle with intense feelings of anxiety, sadness, and anger, which may lead to emotional dysregulation and difficulties in managing these feelings (Brewin et al., 2019). This dysregulation is tied to the neurobiological impact of trauma, particularly alterations in brain regions responsible for emotion processing, such as the amygdala and prefrontal cortex. Physically, women may experience symptoms such as fatigue, insomnia, and heightened physiological responses to stress, which can be detrimental to their overall health (Friedman et al., 2021). Behaviourally, women with PTSD may engage in avoidance behaviours, steering clear of reminders of the trauma, and may also display social withdrawal or difficulty in maintaining relationships due to mistrust or fear (Cloitre et al., 2019). These symptoms collectively impede their ability to function in daily life and often contribute to a cycle of distress that complicates recovery.
Coping strategies among women with PTSD can be both adaptive and maladaptive. Women are more likely to seek social support to manage distress, which is adaptive as the lack of social support is the most consistent predictor of negative outcomes of trauma. While this approach can foster resilience, it can also expose women to risks if their support networks are inadequate or if these relationships reinforce feelings of shame (Tolin & Foa, 2020). This dynamic illustrates the complexity of social support, which can be a double-edged sword in the context of trauma recovery. Furthermore, women have been shown to benefit more from psychotherapy than men in the reduction of PTSD symptoms (Olff, 2017). Recent studies emphasise the importance of understanding the intersectionality of gender, trauma, and mental health. Women may face additional challenges due to societal norms and gender roles that can hinder their ability to seek help or express their needs effectively (Kessler et al., 2017). This underscores the necessity for trauma-informed care that is sensitive to the specific experiences of women, incorporating gender-specific approaches that acknowledge the unique challenges they confront.
With the topic of trauma and PTSD gaining popularity both in research and online discussions, some individuals falsely believe that women are more likely to develop PTSD symptoms and that men do not suffer from trauma. A research paper by Langeland and Olff (2024) analysed 77 different studies that focused on gender differences in regards to trauma. Overall, most of the papers reported gender differences in multiple different areas of psychological and physical trauma.
When faced with self-report and interview questions about experiencing traumatic events, on average men report facing a larger number of traumatising events. However, the participant sample was taken from post-war conflict countries, which contributed to a small diversity of traumatic events overall, as most of them were war-related, which might also contribute to the report of more traumatic events by men (Wilker et al., 2021). In the case of cPTSD (complex PTSD) from various trauma events, no gender difference was observed in symptoms, including psychosis-like ones. However, men reported a higher exposure to physical violence and accidents compared to sexual and emotional assaults, the latter of which were a more common occurrence for women (Ho et al., 2021).
Søegaard et al. (2024) conducted research in a clinic in Norway, investigating various trauma responses, and comparing accidental trauma (AT), for example, accidents or natural disasters, and victimisation trauma (VT), such as prolonged abuse. The results demonstrated that men in the VT group reported more symptoms of negative self-perception than women. Furthermore, when comparing the gender between VT and AT groups, men experienced more difficulties with impulse control, self-perception and relations with others (Søegaard et al., 2021).
Victims of torture or prolonged abuse are at a high risk of developing PTSD. A study that looked at correlations between torture, PTSD symptoms, and gender differences suggests that men are less likely to report sexual abuse, especially if they are homosexuals in a homophobic country, as they can face severe victim blame. The final results reveal that nearly all (98.6%) male patients were registered torture survivors and on average experienced a more diverse range of trauma than women, except in the case of sexual torture (Dalgaard et al., 2021).
Following the establishment of PTSD diagnoses in 1980, the disorder was largely believed inapplicable to young children (Dyregrov and Yule, 2006). However, recent studies estimate that 31% of children experience a traumatic event and 7.8% develop PTSD before the age of 18 (Fariba and Gupta, 2021). Resources such as the Trauma Symptom Checklist for Children (TSCC) and the Screening Tool for Early Predictors of PTSD (STEPP) are often used as additional evidence when evaluating children.
PTSD diagnosis criteria in the DSM-5 vary for children older and younger than six (Fariba and Gupta, 2021). For instance, children above six may show symptoms of PTSD through repetitive play in which they reenact the traumatic event, whereas children below the age of six may experience severe psychological distress in reaction to internal or external stimuli that relate to the event. In addition, the International Classification of Diseases (ICD-11) has PTSD guidelines that differ significantly from those of the DSM-5-TR (Danzi and La Greca, 2016). A study was conducted with children aged 7-11 years old who experienced Hurricane Ike or Hurricane Charley 8-9 months after each event. These children underwent an evaluation using DSM-5, ICD-11, and DSM-IV criteria. Only one third of the children met the appropriate criteria for PTSD across all three tests. Results showed that children who only met the ICD-11 criteria had increased symptom severity but a lower impairment than those who only met the criteria of DSM-5 or DSM-IV. However, overall findings did not demonstrate that one diagnostic system proved more effective than the others.
Children with PTSD are commonly symptomatic in different manners than adolescents and adults. Young children have proven to demonstrate less affective blunting than adults and experience more difficulty self-reporting avoidance reaction symptoms (Dyregrov and Yule, 2006). Children above the age of eight show symptoms more in line with those of adult patients. This is primarily attributed to their growing maturity and ability to reflect on traumatic events, the role they played in the traumatic events, and the consequences the event may have for the future. To a lesser degree, gender is another factor that affects the portrayal of PTSD in children. For instance, boys demonstrated more behavioural symptoms than girls and, similar to adults, young girls are more commonly diagnosed with PTSD than young boys.
The Different Socio-Economic Factors Which Affect PTSD
PTSD is affected by various socio-economic factors. A person’s access to healthcare, social status, level of education, and financial status are all factors that influence the development of PTSD (Nurius et al., 2013).
Access to healthcare and an individual’s social status are closely intertwined. Those who are financially better off have greater possibilities when it comes to healthcare, allowing them to consult with higher-ranking doctors and afford necessary medications without hesitation. In contrast, individuals with a lower social status, who have limited financial resources, have to be more careful with their spending and prioritise spending money on certain things. Such prioritisation would likely result in emphasis on spending for essentials, such as food and accommodation, over treatments for PTSD, such as therapy and medication. Refugees’ and asylum-seekers’ access to healthcare is often limited due to language barriers, financial constraints, and a lack of trust in healthcare providers (Nurius, Uehara and Zatzick, 2013). This sets a major problem as these groups of people are often affected by psychological trauma due to their pre-/post-migration experiences (Due et al., 2020). PTSD more often affects people with migrational backgrounds, as many have had to endure traumatic events. However, these people are often the ones for whom it is harder to get medical help/treatments, which contributes to explaining why certain social groups are affected more by PTSD. A person’s social support and living conditions also play major roles in the development of PTSD. These factors can either enhance or hinder mental health outcomes (Tran et al., 2013).
Personal characteristics, such as level of education, can influence one’s degree of risk for developing post-traumatic stress disorder. Higher levels of education often correlate with better awareness of mental health issues, including PTSD. Educated individuals may be more likely to recognise the symptoms of PTSD and seek help promptly. They may also have wider access to resources and information about coping mechanisms, which can have an effect on the impact of trauma. Additionally, education can lead to improved employment opportunities, which in turn can provide individuals with better healthcare access and social support networks (Brennstuhl et al., 2015). One’s level of education not only impacts one’s understanding and perception of the problem, but also of the ability to contest it.
Poverty is another significant socio-economic factor that can aggravate PTSD. The burden of trauma is not equally distributed among all groups of societies and often disproportionately affects poorer populations. Sociodemographic factors have been shown to be related to both PTSD and pain, with lower socio-economic position (SEP) – quantified using income, employment status, educational attainment, and neighbourhood poverty level – associated with more severe PTSD symptoms and worse pain outcomes (Davies et al., 2009; Phifer et al., 2011). Individuals living in poverty are often exposed to higher levels of stress and trauma due to unstable living conditions, violence, and limited access to healthcare and social services. These conditions can increase the likelihood of experiencing traumatic events and can make it more challenging to recover from them. Poverty can limit access to mental health care, as individuals may not have the financial means to afford therapy or medication (Diez Roux and Mair, 2010; Kind and Buckingham, 2018). The chronic stress associated with poverty can intensify PTSD symptoms, creating a cycle where financial strain worsens mental health, and untreated PTSD inhibits an individual’s ability to improve their economic situation.
How Does PTSD Affect Sleep?
Sleep Disturbances, PTSD, and the Brain
Sleep disturbances, such as nightmares and insomnia, are commonly occurring symptoms in PTSD individuals (El-Solh, 2018; Marike Lancel, 2021). Insomnia is mostly caused by hyperarousal, as the individual cannot relax. This could be the effect of experiencing a situation which required the individual to be in constant alertness. Furthermore, the stress of not being able to fall asleep may lead to maladaptive sleep behaviours. Nightmares lead to awakenings and are more like vivid dreams depicting past trauma (Pacheco, 2021). PTSD individuals are consistently in fight-or-flight mode during sleep. It is suggested that these factors occur due to the brain’s processing of fearful memories. In a traumatic event, the brain activates a negative response stimulus, which, if strong enough, could activate violent reactions to similar stimuli long after the trauma (Pacheco, 2021).
Nightmares, also known as REM parasomnias, often reflect the traumatic event the individual was exposed to, or a time when the individual’s emotional and physical sense of safety was threatened (El-Solh, 2018). These nightmares and insomnias are modulated by brain areas which are affected in PTSD, such as the hippocampus, the amygdala and locus coeruleus. The irregularities in activities in these brain regions are regulated by the neurochemical imbalance in the serotonin, dopaminergic and noradrenergic pathways (El-Solh, 2018; Nardo et al., 2015).
Sleep fragmentation reduces neurogenesis, which causes a neuronal loss in the hippocampus. Structural changes have also been found near the orbitofrontal cortex, where large changes in volume were seen in the ACC (anterior cingulate cortex). The severity of insomnia also seems to be connected with the volume, as there were connections between grey matter volume in the prefrontal cortex and insomnia severity (El-Solh, 2018). Recent neuroimaging data demonstrates that PTSD individuals show increased locus coeruleus activity (which is associated with fear and stress processing, memory, and pain modulation, among other processes) during the REM sleeping stage (Walker, 2014). This suggests that those with PTSD experience an abnormally high level of fear and stress processing during sleep. This abnormal activity could also be related to the experience of nightmares, due to the involvement of the locus coeruleus in memory processing.
Nardo et al. (2015) examined the relationships between neurobiological differences in PTSD and sleep disturbances. They found that higher sleep disturbances were related to reduced grey matter volume (GMV) in the hippocampus, amygdala, anterior cingulate, and insula; decreased regional cerebral blood flow (rCBF) in the anterior cingulate; and increased rCBF in the midbrain, insula, and precuneus. These neurobiological areas are also those which have been found to be altered in people with PTSD. As a result, they concluded that the experience of sleep disturbances is significantly related to PTSD, and may be attributable to the effects that PTSD can have on neurological structures and their functions.
Reduced grey matter volume (GMV) in the hippocampus, amygdala, anterior cingulate, and insula; decreased regional cerebral blood flow (rCBF) in the anterior cingulate; and increased rCBF in the midbrain, insula, and precuneus were all related to higher sleep disturbances. Usual sleep disturbances are associated with reduced GMV in the anterior limbic/paralimbic; PTSD sensitive brain regions, and changes in the regions’ functions, are associated with REM sleep control (Nardo et al., 2015). Studies have found that the hippocampus also plays a role in sleep disturbances, with findings of bilaterally reduced hippocampal volume in individuals who suffer from insomnia. On top of that, studies have found that individuals with PTSD are more likely to experience Periodic Limb Movement Disorder, which causes limb movements during sleep and can result in decreased sleep quality. This could contribute to the higher number of arousals/awakenings experienced by individuals with PTSD (Lancel, 2021). Such parasomnias (including disruptive nocturnal behaviours and complex body movements) do not exclusively occur in REM stages of sleep, but can also occur in non-REM stages. However, individuals do not remember the experiences happening during the non-REM stages (Lancel, 2021). Therefore, individuals with PTSD may experience more sleep disturbances than they realise and report.
The neuromodulatory pathways in the brain may contribute to the link between PTSD and sleep disturbance. For example, noradrenergic projections from the locus coeruleus could contribute to the hyperarousal seen in both PTSD and sleep disturbances, given that insomnia, nightmares and other sleep disorders are caused by the state of hyperarousal and recurring disruption during REM sleep (MLancel, 2021).
Medications for PTSD Sleep Disturbance
Concerning PTSD treatments, trauma-focused therapies, such as CPT, PE, and EMDR, are considered the most effective, though medications are still used (Schrader and Ross, 2021; Yehuda et al., 2015). It is, however, crucial to investigate the effects of treatments on sleep disturbances, as nightmares and insomnia can affect the development and maintenance of PTSD and can affect distress, reactivity to emotional cues, and general health (Nappi et al., 2012; Weber and Wetter, 2021). Moreover, suppressive symptoms can disrupt daily functioning and can increase the difficulty for a person to maintain healthy relationships.
Despite psychotherapy being recommended as first-line treatment (especially cognitive behavioural therapy and exposure-based therapy) for PTSD, there are also two types of SSRIs (sertraline and paroxetine) which are suggested by the FDA for use as pharmacological therapy (Yehuda et al. 2015; Zaretsky et al., 2024). Other medications, however, are prescribed off-label based on new research on the neuroscience of PTSD (Yehuda et al. 2015; Marazziti et al., 2023). Specifically, concerning the treatment of sleep disruption in PTSD, some antidepressants (such as amitriptyline) might have a light positive effect on insomnia, but its effects haven’t been studied a lot and they could also have adverse effects that should be taken into consideration (Weber and Wetter, 2021; Lappas et al., 2024). Z-drugs and benzodiazepines have also been shown to have some positive effects in the treatment of insomnia, but their addictive potential makes clinicians avoid them for long-term treatment (Weber and Wetter, 2021; Lappas et al., 2024). There are other drugs that have been studied as possible forms of treatment for PTSD, such as mirtazapine (which would specifically help to reduce nightmares), but evidence about their efficacy is limited (Marazziti et al., 2023). All the drugs used as treatments for insomnia in the guidelines of American Academy of Sleep Medicine (AASM) are not singularly recommended as more than “weak”, which implies an uncertainty concerning the drug’s effectiveness for insomnia. However, this does not necessarily imply unsuccess (Weber and Wetter, 2021).
It is important to note that all the medications currently prescribed to treat PTSD are actually drugs which were first used to treat other disorders, and there has yet to be a drug that has been developed specifically for PTSD (Zaretsky et al., 2024). The response rate of PTSD to pharmacological treatments remains low (Marazziti et al., 2023). This could be due to high levels of comorbidity in PTSD (with anxiety and depression often manifesting alongside PTSD) and the high level of diversity in PTSD symptoms.
Role of Noradrenaline in PTSD
Noradrenaline, also known as norepinephrine, is a well-known catecholamine, which is a type of neurohormone (Medline Plus, 2023). Noradrenaline is both a hormone and a neurotransmitter. As a neurotransmitter, noradrenaline has the vital role of being a chemical messenger that helps transfer nerve signals to nerve endings and to other nerve, gland and muscle cells. As a hormone, noradrenaline is released by the adrenal glands and is located on the surface of each kidney (Cleveland Clinic, 2022). Noradrenaline is implicated in PTSD, and is suggested to enhance the processing of the traumatic event (Gören and Cabadak, 2015). It is common for individuals with PTSD to experience hyperarousal and hypervigilance (Southwick et al., 1999). Given that arousal is impacted by noradrenaline activity, abnormalities in noradrenergic pathways in PTSD might explain this hyperarousal and hypervigilance in PTSD.
Given noradrenline’s role in PTSD, medications used in treating PTSD often target noradrenaline activity. A study conducted by Director Masatake Kurita of Wakamiya Hospital in Japan explores the important role of noradrenaline in the treatment of Bipolar Depression (BD), where patients experience spurs of intense and sometimes aggressive emotions. They found that antidepressants, which increase levels of noradrenaline, result in a higher risk of the patient switching from their depressive state to a manic state. Therefore, such antidepressants can worsen the condition of patients with bipolar depression, rather than helping them. Many of the same antidepressants used to treat bipolar depression have also been used to treat PTSD. It follows that the use of these antidepressants, which induce high noradrenaline levels, in treating PTSD could pose a risk of worsening the patient’s state or even re-triggering some of the patient’s traumas.
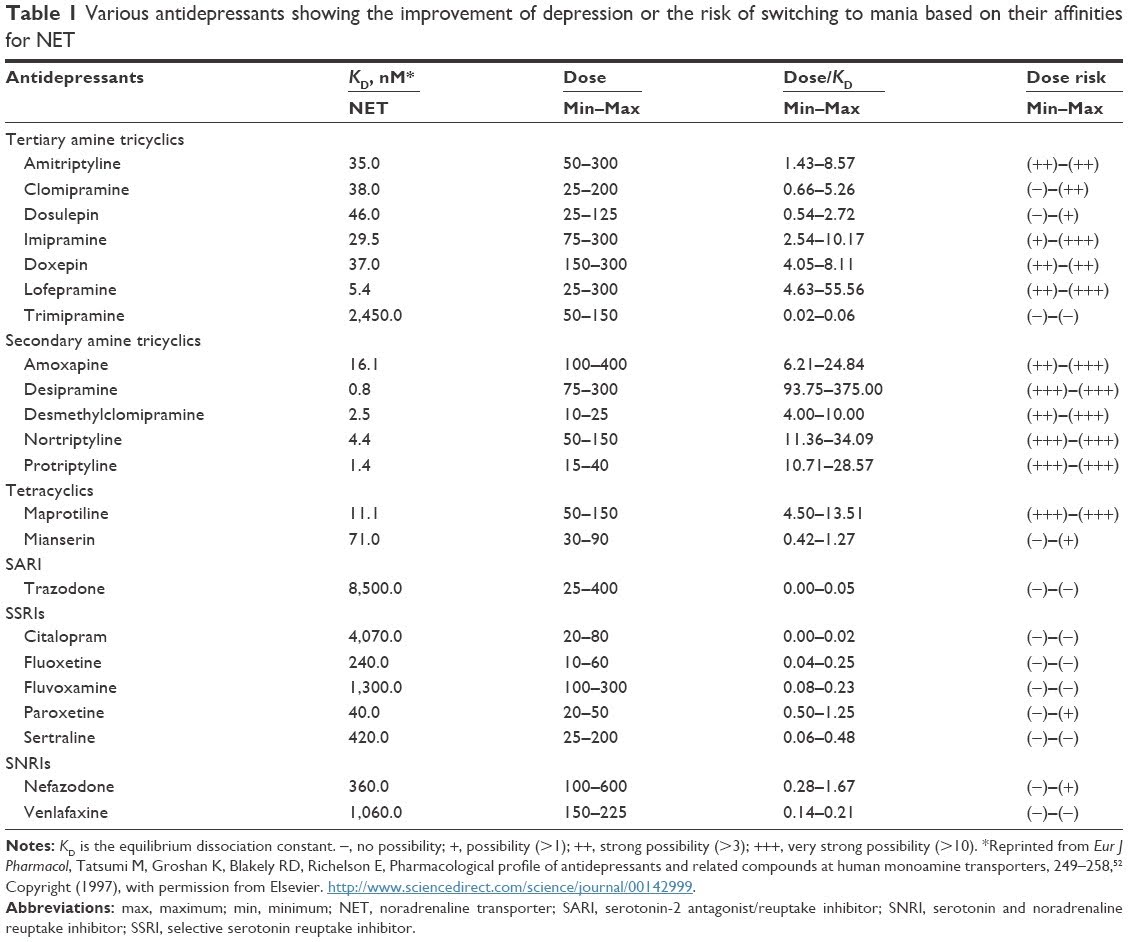
Table 1: This table shows how more noradrenaline (measured in NET) creates a higher chance of the patient changing from their depressive state to their manic state, as shown in the table by the (+) and (-) symbols.
Outside of noradrenaline, other neurotransmitters (including other catecholamines, serotonin, and peptide and opioid neurotransmitters) have also been implicated in PTSD development. All of these neurotransmitters are located in brain circuits that regulate responses to high fear and high stress situations (Sherin and Nemeroff, 2011).
Discussion
PTSD affects individuals who have been exposed to trauma. Symptoms of PTSD include sleep disturbances, hypervigilance, flashbacks that reflect their trauma, poor concentration, and irritability affecting their daily life (Yehuda et al., 2015; National Institute of Mental Health, 2023). Individuals suffering from PTSD are always on high alert and their brains are always in fight-or-flight mode (Yehuda et al., 2015; Schrader and Ross, 2021). During the traumatic event, the brain stimulates a negative response stimulus leading to various symptoms and consequences for the individual later on (Pacheco, 2021). We must also keep in mind that external factors like socio-economic factors may also affect one’s likelihood of developing PTSD (Due et al., 2020).
The impacts and causes of PTSD are different between women and men. PTSD impacts more women than men in general since women are more prone to experience sexual assault and other scenarios like that (National Institute of Mental health, 2023). However, more investigations are currently being run to understand whether or not this is the only reason. Another topic we must be careful with is that PTSD is different based on the individual’s age. For example, we found that there are different diagnosing criteria for children under the age of six (Fariba and Gupta, 2021). Further investigations could explore whether toddlers can develop PTSD, and whether they would experience the same symptoms as older children.
Current research on personal differences in PTSD symptoms is diverse, usually exploring specific scenarios. This results in a large variety of information, but it’s easy to get misled by non-generalisable data. For example, specific trauma symptoms which have been found in children in single-parent households in Eastern Europe may not be applicable to all children who experience a traumatic event. Therefore it’s important to draw correct conclusions from given research and to be cautious when combining multiple different points from several scientific papers.
As we’ve discussed, a PTSD individual’s brain is always on high alert mode, which leads to sleep disturbances. In this paper, we’ve mainly analysed the experiences of nightmares and insomnia. When having insomnia, the individual’s brain cannot rest due to the fear-inducing memories that are projected during sleep, and the brain automatically remains in a fight-or-flight state, thus rendering their nights sleepless (Pacheco, 2021). Nightmares project the individual’s traumatic event, or when the individual felt threatened in the sense of safety, during sleep (El-Solh, 2018). Sleep disturbances mainly occur during REM sleep and have been associated with neurobiological differences in the hippocampus, amygdala, and locus coeruleus. These are all regions which are PTSD-sensitive regions. However, investigations for direct correlations between sleep disturbances and PTSD are still ongoing (Lancel, 2021).
From the research paper, we’ve seen that noradrenaline plays an important role in PTSD. Noradrenaline can both be a hormone as well as a neurotransmitter (Cleveland Clinic, 2022). It is responsible for the fight-or-flight response and for the security system, as it modulates arousal. However, we still have a lot to learn and research about the exact role of noradrenaline since we know so little about it.
We have many treatments to heal sleep disturbances and PTSD. Psychological treatments such as CBT and exposure-based therapies (e.g., Cognitive Processing Therapy, Prolonged Exposure, and Eye Movement Desensitization and Reprocessing) are mostly considered the best form of first-line treatment. Medications such as SSRIs are still used. However, a drug specifically for PTSD has yet to be designed (Yehuda et al. 2015; Zaretsky et al., 2024). Further exploration of PTSD could help our development of treatments to target the symptoms experienced in PTSD.
Bibliography
Abdallah, C.G., Averill, L.A., Akiki, T.J., Raza, M., Averill, C.L., Gomaa, H., Adikey, A. and Krystal, J.H. (2019). The neurobiology and pharmacotherapy of posttraumatic stress disorder. Annual Review of Pharmacology and Toxicology, [online] 59(1), pp.171–189. doi:https://doi.org/10.1146/annurev-pharmtox-010818-021701.
Armour, C., Contractor, A.A., Palmieri, P.A. and Elhai, Jon.D. (2014). Assessing latent level associations between PTSD and dissociative factors: is depersonalization and derealization related to PTSD factors more so than alternative dissociative factors? Psychological Injury and Law, 7(2), pp.131–142. doi:https://doi.org/10.1007/s12207-014-9196-9.
Bremner, J.D. (2006). Traumatic stress: effects on the brain. Dialogues in Clinical Neuroscience, [online] 8(4), pp.445–461. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181836/#:~:text=Brain%20regions%20that%20are%20felt.
Burgland, C. (2024). What Is Hyperarousal in PTSD? Verywell Health. Available at: https://www.verywellhealth.com/hyperarousal-in-ptsd-5219152#:~:text=As%20its%20name%20suggests%2C%20hyperarousal.
Center for Substance Abuse Treatment (2014). DSM-5 Diagnostic Criteria for PTSD. [online] National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK207191/box/part1_ch3.box16/.
Cleveland Clinic (2022). Norepinephrine: What it is, function, deficiency & side effects. [online] Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/articles/22610-norepinephrine-noradrenaline.
Cleveland Clinic (2023). The amygdala: A small part of your brain’s biggest abilities. [online] Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/body/24894-amygdala.
Compean, E. and Hamner, M. (2019). Posttraumatic stress disorder with secondary psychotic features (PTSD-SP): Diagnostic and treatment challenges. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 88, pp.265–275. doi:https://doi.org/10.1016/j.pnpbp.2018.08.001.
Dalgaard, N.T., Bjerre, K. and Thøgersen, M.H. (2021). Twenty seven years of treating survivors of torture and organized violence – associations between torture, gender and ethnic minority status among refugees referred for treatment of PTSD. European Journal of Psychotraumatology, 12(1), p.1904712. doi:https://doi.org/10.1080/20008198.2021.1904712.
Danzi, B.A. and La Greca, A.M. (2016). DSM-IV, DSM-5, and ICD-11: Identifying children with posttraumatic stress disorder after disasters. Journal of Child Psychology and Psychiatry, 57(12), pp.1444–1452. doi:https://doi.org/10.1111/jcpp.12631.
Due, C., Green, E. and Ziersch, A. (2020). Psychological trauma and access to primary healthcare for people from refugee and asylum-seeker backgrounds: a mixed methods systematic review. International Journal of Mental Health Systems, 14(1). doi:https://doi.org/10.1186/s13033-020-00404-4.
Dyregrov, A. and Yule, W. (2006). A review of PTSD in children. Child and Adolescent Mental Health, [online] 11(4), pp.176–184. doi:https://doi.org/10.1111/j.1475-3588.2005.00384.x.
Fariba, K. and Gupta, V. (2021). Posttraumatic Stress Disorder In Children. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK559140/.
Gören, M.Z. and Cabadak, H. (2015). Noradrenaline and Post-traumatic Stress Disorder. Comprehensive Guide to Post-Traumatic Stress Disorder, pp.1–16. doi:https://doi.org/10.1007/978-3-319-08613-2_26-1.
Ho, G.W.K., Hyland, P., Karatzias, T., Bressington, D. and Shevlin, M. (2021). Traumatic life events as risk factors for psychosis and ICD-11 complex PTSD: a gender-specific examination. European Journal of Psychotraumatology, 12(1). doi:https://doi.org/10.1080/20008198.2021.2009271.
Kessler, R.C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E.J., Cardoso, G., Degenhardt, L., de Girolamo, G., Dinolova, R.V., Ferry, F., Florescu, S., Gureje, O., Haro, J.M., Huang, Y., Karam, E.G., Kawakami, N., Lee, S., Lepine, J.P., Levinson, D. and Navarro-Mateu, F. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(sup5). doi:https://doi.org/10.1080/20008198.2017.1353383.
Langeland, W. and Olff, M. (2024). Sex and gender in psychotrauma research. European Journal of Psychotraumatology, 15(1). doi:https://doi.org/10.1080/20008066.2024.2358702.
McManus, S., Meltzer, H., Brugha, T., Bebbington, P.E. and Jenkins, R. (2009). Adult psychiatric morbidity in England: results of a household survey. [online] openaccess.city.ac.uk. Available at: https://openaccess.city.ac.uk/id/eprint/23647/.
Medline Plus (2023). Catecholamine Tests: MedlinePlus Medical Test. [online] medlineplus.gov. Available at: https://medlineplus.gov/lab-tests/catecholamine-tests/#:~:text=Catecholamines%20are%20hormones%20made%20by.
National Institute of Mental Health (2023). Post-traumatic stress disorder. [online] National Institute of Mental Health. Available at: https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd.
Nurius, P.S., Uehara, E. and Zatzick, D.F. (2013). Intersection of stress, social disadvantage, and life course processes: reframing trauma and mental health. American Journal of Psychiatric Rehabilitation, 16(2), pp.91–114. doi:https://doi.org/10.1080/15487768.2013.789688.
Nutt, D. and Malizia, A. (2004). Structural and functional brain changes in PTSD 11. Journal of Clinical Psychiatry, [online] 65(1). Available at: https://www.psychiatrist.com/read-pdf/20094/.
Porrey, M. (2023). Conditions Exposure Therapy Could Benefit. [online] Verywell Health. Available at: https://www.verywellhealth.com/exposure-therapy-7975314.
PTSD UK(7AD). The Science and Biology of PTSD – PTSD UK. [online] PTSD UK. Available at: https://www.ptsduk.org/what-is-ptsd/the-science-and-biology-of-ptsd/#:~:text=Someone%20who%20has%20PTSD%20or.
Ressler, Kerry.J., Berretta, S., Bolshakov, V.Y., Rosso, I.M., Meloni, E.G., Rauch, S.L. and Carlezon, W.A. (2022). Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits. Nature Reviews Neurology, 18(5), pp.273–288. doi:https://doi.org/10.1038/s41582-022-00635-8.
Rumball, F., Happé, F. and Grey, N. (2020). Experience of trauma and PTSD symptoms in autistic adults: Risk of PTSD development following DSM‐5 and non‐DSM‐5 traumatic life events. Autism Research, 13(12). doi:https://doi.org/10.1002/aur.2306.
Schrader, C. and Ross, A. (2021). A Review of PTSD and Current Treatment Strategies. Missouri medicine, [online] 118(6), pp.546–551. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8672952/#sec-a.f.btitle
Sherin, J.E. and Nemeroff, C.B. (2022). Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Trauma, Brain Injury, and Post-traumatic Stress Disorder, [online] 13(3), pp.263–278. doi:https://doi.org/10.31887/dcns.2011.13.2/jsherin.
Søegaard, E.G.I., Kan, Z., Koirala, R., Hauff, E. and Thapa, S.B. (2021). Gender differences in a wide range of trauma symptoms after victimisation and accidental traumas: a cross-sectional study in a clinical setting. European Journal of Psychotraumatology, 12(1). doi:https://doi.org/10.1080/20008198.2021.1975952.
Tran, U.S., Glück, T.M. and Lueger-Schuster, B. (2013). Influence of personal and environmental factors on mental health in a sample of Austrian survivors of World War II with regard to PTSD: is it resilience? BMC Psychiatry, [online] 13(1). doi:https://doi.org/10.1186/1471-244x-13-47.
Wilker, S., Kolassa, S., Ibrahim, H., Rajan, V., Pfeiffer, A., Catani, C. and Kolassa, I. (2021). Sex differences in PTSD risk: evidence from post-conflict populations challenges the general assumption of increased vulnerability in females. European Journal of Psychotraumatology, [online] 12. doi:https://doi.org/10.1080/20008198.2021.1930702.
Yehuda, R., Hoge, C. W., McFarlane, A. C., Vermetten, E., Lanius, R. A., Nievergelt, C. M., Hobfoll, S. E., Koenen, K. C., Neylan, T. C., and Hyman, S. E. (2015). Post-traumatic stress disorder. Nature Reviews. Disease primers, 1, 15057. https://doi.org/10.1038/nrdp.2015.57




